The questions we asked were as followed:
- January- Do you share inhalation kits (pipes)?
- February- Would you use a safe consumption site?
- March- What do you do for needles/supplies when we're closed?
- April- Have you ever used Naloxone on someone?
- May- Have you ever gotten an abscess?
- June- Who introduced you to drugs?
- July - Do you use alone?
- August- What's your drug of choice?
- September- Could you get through the day without using?
- October- Do you mix drugs?
- November- What do you do with your discarded needles or broken pipes?
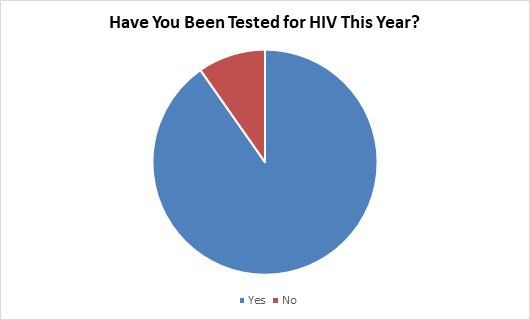
- December- Have you been tested for HIV?
People were very open with their answers, even to the point of going into detail and telling our staff their story. By providing a safe space, being anonymous and having consistent staff, needle exchange clients are more likely to trust us.
The responses from PWUD have been informative which have helped in relationship building as well as enhance our programs to meet the needs of our clients.
In 2021, we will take this data as a needs assessment and turn what we have learned into where we need to focus. This could include: increased youth education on injection drug use, working with our NEP clients in a way they will understand, and creating awareness events for the public.
January
23 Females said yes (19 were Aboriginal/ 4 were Caucasian). 7 Females said no (5 were Aboriginal/ 2 were Caucasian).
34 Males said yes (21 were Aboriginal/ 12 were Caucasian/1 was Other). 36 Males said no (30 were Aboriginal/ 6 were Caucasian).
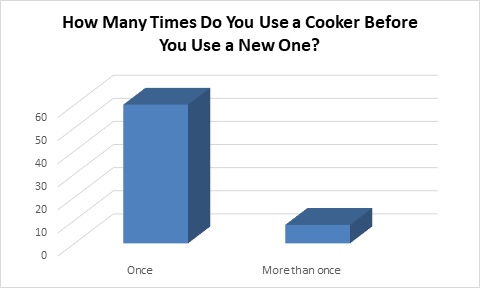
Smoking crack or crystal meth from a pipe can cause burns and cuts on lips, inside of the mouth, or on the fingers. HCV can be transmitted from person to person through the presence of blood (seen or unseen). To prevent this, mouth pieces are provided to encourage people not to share as well as protect them from burning their lips.
One person remarked that he used to share pipes until he started receiving kits from APSS and read the educational materials we provide. Each kit has a pamphlet on safer Crack/Meth smoking, overdose information, and HIV/HCV risks when sharing pipes.
Another person specified that they share pipes but would never share needles because of the risk of HIV. They were informed that sharing pipes had a low chance of transmitting HIV but there was still a risk. Sharing pipes has a high risk to transmit HCV.
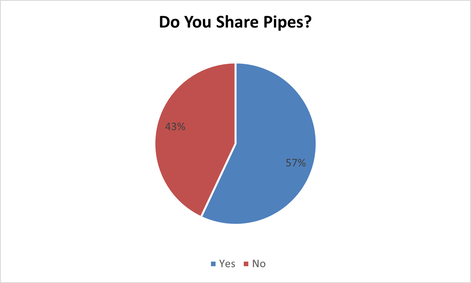
Feburary
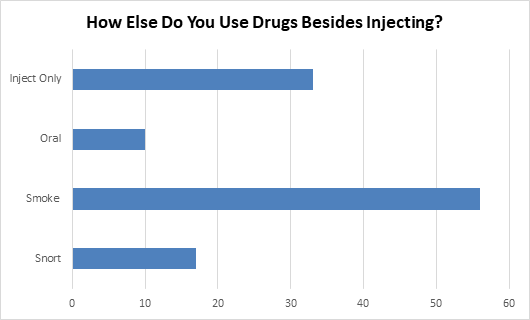
Of the people asked, 33% only use injection drugs, 10% only smoke their drugs, and the remaining 57% use both injection and inhalation drugs. This greatly impacted the answers for the question as many people have heard of “safe injection sites” but not SCS’s where any form of drug can be safely taken. After clarification was given that many SCS’s not only have safe smoking rooms as well as injection rooms, they also have staff to assist with overdoses, abscesses, referrals to treatment/detox, and opioid substitution therapy like Methadone/Suboxone, many people changed their answers and grew excited at the thought of Regina one day having such a service.
20 Females said yes (19 were Aboriginal/ 1 was Caucasian). 7 Females said no (5 were Aboriginal/ 2 were Caucasian).
43 Males said yes (32 were Aboriginal/ 11 were Caucasian). 8 Males said no (2 were Aboriginal/ 6 were Caucasian).
2 people who answered no to the question are from out of town (approx. 2 hours drive away), however, another two people who answered yes say they travel to Edmonton to use their safe injection site (an 8 hour drive from Regina).
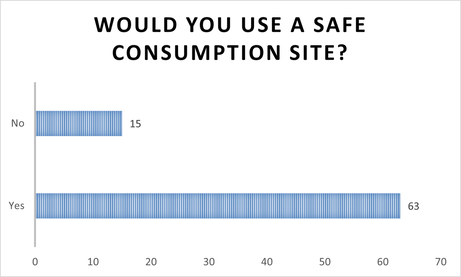
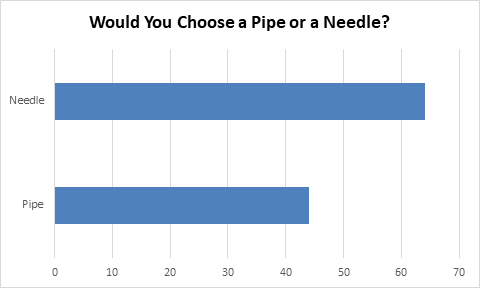
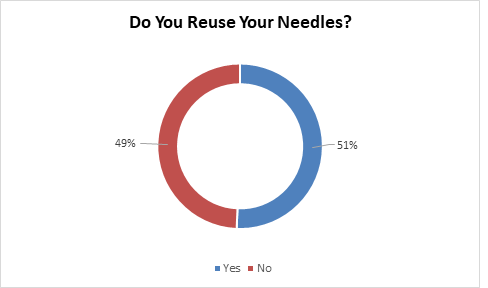
march
12 Females said they reuse old needles (8 were Aboriginal/ 4 were Caucasian). 12 Females said they borrow from family/friends (All were Aboriginal). 4 Females said they stock up (All were Aboriginal). 8 Females said they go to another site (7 were Aboriginal/ 1 was Caucasian). 3 Females said they wait till we are open (All were Aboriginal).
11 Males said they reuse old needles (4 were Aboriginal/ 7 were Caucasian). 23 Males said they borrow from family/friends (17 were Aboriginal/ 5 were Caucasian/ 1 was Other). 13 Males said they stock up (9 were Aboriginal/ 4 were Caucasian). 14 Males said they go to another site (11 were Aboriginal/ 3 were Caucasian). 10 Males said they wait till we are open (9 were Aboriginal/ 1 was Caucasian).
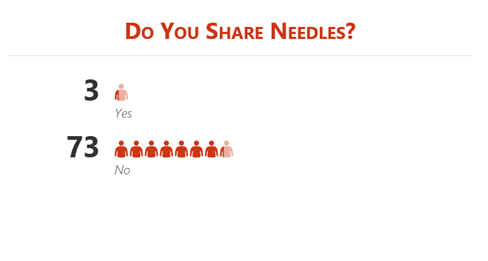
Over 50% of people asked, reported that when we are not open, they reuse their old needles (especially on “Reuse Sundays”) and borrow/share from family and friends.
Currently in Regina, there are 3 places you can get needles and/or exchange: APSS, Downtown at the Sexual Health Clinic, and from the Street Project Van. No services are available after 8pm or on Sunday. Since many people who use drugs are not on a 9-5 schedule, accessing harm reduction supplies can be difficult. Clients commented, during the survey, that it would be better if APSS was open 7 days a week to get their harm reduction supplies.
On May 10th, APSS began opening on Sundays for 4 hours changing APSS’ schedule to be open Tuesday-Sunday with Monday covered by the Downtown location.
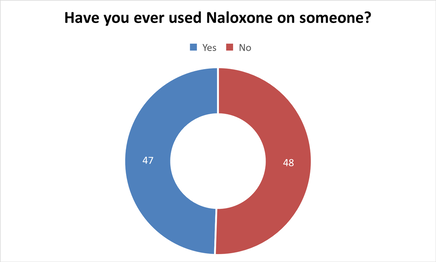
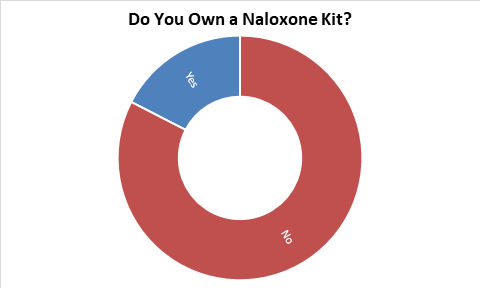
April
24 Females said yes (18 were Aboriginal/ 5 were Caucasian/1 was Other). 16 Females said no (12 were Aboriginal/ 4 were Caucasian).
23 Males said yes (16 were Aboriginal/ 7 were Caucasian). 31 Males said no (24 were Aboriginal/ 6 were Caucasian/1 was Other).
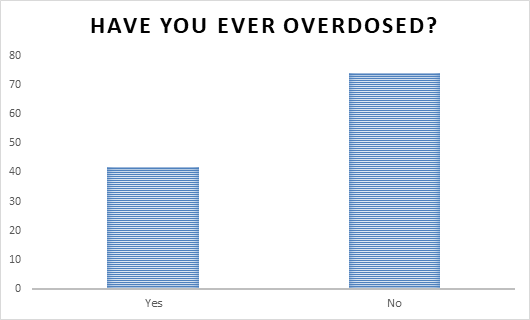
According to a Leader Post article (https://leaderpost.com/news/local-news/number-of-drug-overdoses-now-at-208-say-regina-police/),“So far this year, the Regina Police Service (RPS) has reported 208 overdoses. The total number for 2019 was 82. Of the 208 overdoses, police have attended 103 and administered Narcan on 24 occasions. There have been 11 confirmed fatalities due to overdoses, and nine unconfirmed fatalities.”
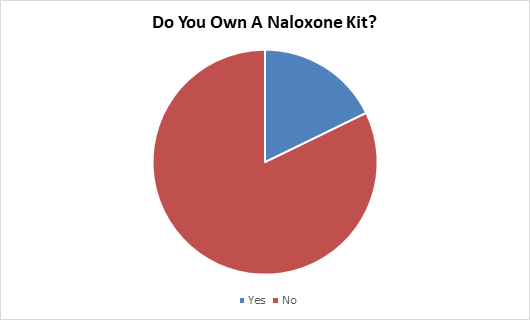
From January to April, APSS distributed 495 Naloxone kits, in comparison to the full year of 2019, where we distributed 353 kits. Of the 495, 203 were used in an overdose situation. The main drug used when our clients are responding to an overdose is Fentanyl.
All APSS staff have been trained and will be able to train anyone interested in Naloxone. The training, depending on those being trained, takes 15 minutes and trains individuals on how to administer the drug, how to identify an overdose, and overdose prevention. APSS staff have never administered Naloxone at the office, however on April 23rd, staff responded to a client having a Crystal Meth overdose in the exchange. Staff knew Naloxone would not be effective and followed 911’s steps to help the client through the overdose as there is no cure for a Crystal Meth overdose.
A quote from a client trained on Naloxone: “I think y'all are doing such a great job. There has been times where people have been right next to me and I didn't know what to do but now I feel I can save a life.”
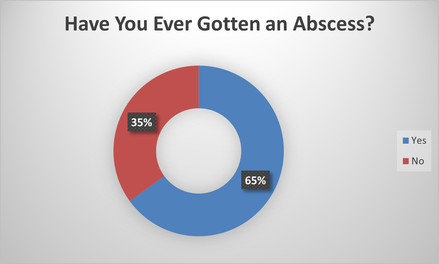
May
21 Females said yes (17 were Aboriginal/ 4 were Caucasian). 13 Females said no (11 were Aboriginal/ 2 were Caucasian).
43 Males said yes (32 were Aboriginal/ 11 were Caucasian). 22 Males said no (19 were Aboriginal/ 2 were Caucasian/1 was Other).
Studies have shown a connection between abscesses and HIV. According to the NHS, “things that increase the likelihood of an abscess developing can include having a weakened immune system – this could be because of a medical condition such as HIV, or a treatment such as chemotherapy”. Cutaneous, relating to or affecting the skin, manifestations of HIV results from the HIV infection itself or from opportunistic disorders secondary to the decline in the immune system.
Clients are reminded that consistent use of clean needles and swabbing before injecting can reduce the risk of developing an abscess from IV drug use but will not eliminate it entirely. Any time the skin is pierced with a foreign object, the risk of infection will remain. Clients are also reminded that abscesses can happen anywhere on the body, not just where they have injected. Many clients have asked for abscess kits from our exchange. We do not have such an item but when asked, clients explained that the kits would contain a cleaning solution like hydrogen peroxide and band aids. Any client who asks for a kit and/or has an abscess is referred to a doctor as draining an abscess alone is dangerous and many abscesses need to be treated with antibiotics.
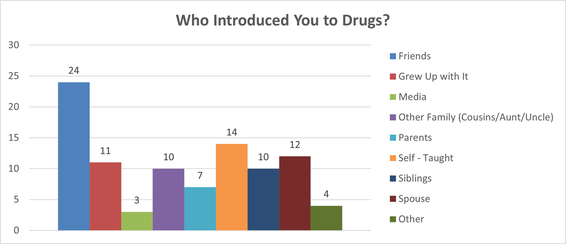
June
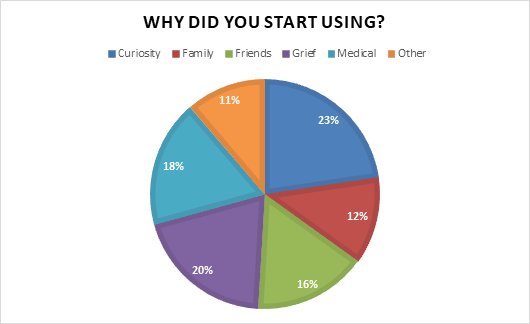
11 Females said friends (All were Aboriginal). 7 Females said they grew up with it (5 were Aboriginal/2 were Caucasian). 2 Females said other family such as cousins/aunts/uncles (Both were Aboriginal). 2 Females said their parents (Both were Aboriginal). 2 Females said self-taught (Both were Aboriginal). 5 Females said their siblings (3 were Aboriginal/ 2 were Caucasian). 7 Females said their spouse (All were Aboriginal). 2 Females said other (Both were Aboriginal).
13 Males said friends (5 were Aboriginal/ 8 were Caucasian). 4 Males said they grew up with it (All were Aboriginal). 3 Males said the media (2 were Aboriginal/1 was Caucasian). 8 Males said other family such as cousins/aunts/uncles (6 were Aboriginal/ 2 were Caucasian). 5 Males said their parents (4 were Aboriginal/ 1 was Caucasian). 12 Males said self-taught (9 were Aboriginal/ 3 were Caucasian). 5 Males said their siblings (All were Aboriginal). 4 Males said their spouse (All were Aboriginal). 2 Males said other (1 was Aboriginal/ 1 was Caucasian).
1 person identifying as Non-Binary said spouse.
For the clients who answered self- taught, many used trial and error while others taught themselves from watching in person or on the internet.
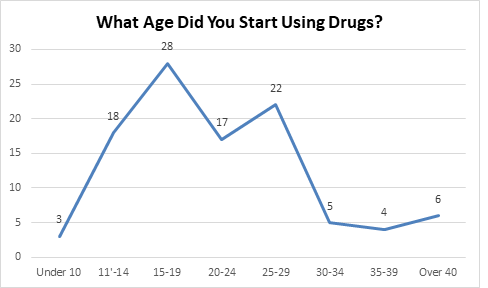
Clients talked about being born addicted, starting at 11/12 years old, being teased by their family for having “virgin veins”, a mother injecting her child at 17 years old because the rest of their family uses, using it to have power/sexual control, or being curious but then not expecting to like it or become addicted to it.
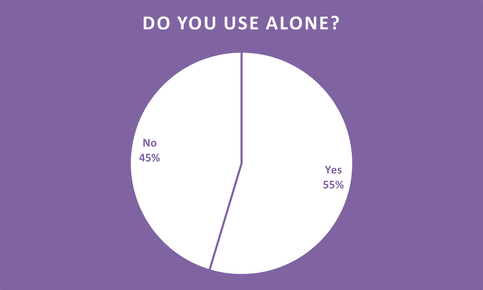
July
23 Females said yes (21 were Aboriginal/ 2 were Caucasian). 20 Females said no (14 were Aboriginal/ 6 were Caucasian).
30 Males said yes (18 were Aboriginal/ 12 were Caucasian). 24 Males said no (17 were Aboriginal/ 7 were Caucasian).
Each client who answered our survey were given overdose prevention education to ensure that they were aware of the risks of using alone with the rise in Fentanyl. Many client’s self-identified that they do not use opioids, however, we still encouraged them to have a safety plan as it is still possible to overdose on any substance. One client no longer uses Fentanyl after keeping a journal of all his friends who have passed from Fentanyl overdoses. He has 18 names written down to date. Another client used to use alone until two nights before he answered the survey, he went to bed after using and woke up to his wife responding to his overdose. Now they have a “use plan” which involves using when someone is around and having Naloxone available. Clients were also given the option to get trained in Naloxone and receive a kit. 189 Naloxone kits given out in July.
On Overdose Awareness Day, August 31st, APSS’ education team trained 48 members of the public in Naloxone. As the office is not open on Mondays, APSS held an office event on September 1st in lieu of Overdose Awareness Day. 16 clients received education of overdose prevention, Naloxone kits and training, as well as coffee and snacks.
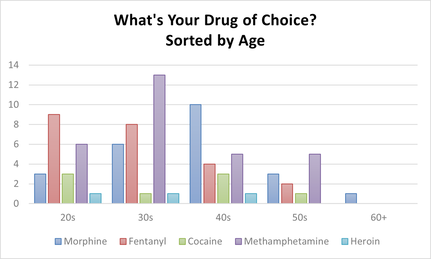
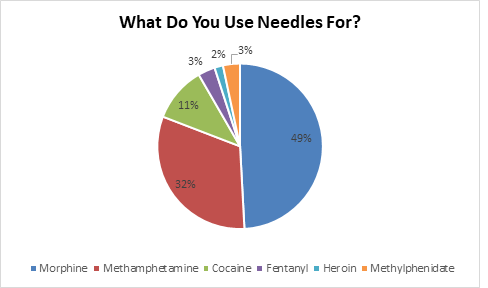
August
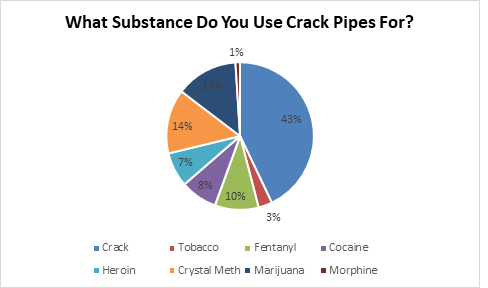
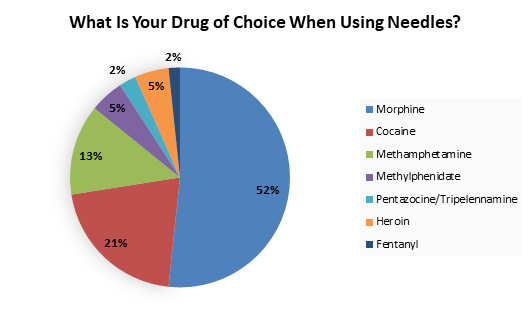
Listed on the graph are the medical drug names but in the Needle Exchange we received the following drug slang: Down, Side, Beads, Billy Eights, Coke, and Jib.
8 Females said Morphine (7 were Aboriginal/ 1 was Caucasian). 10 Females said Fentanyl (7 were Aboriginal/ 3 were Caucasian). 1 Female said Cocaine (She was Aboriginal). 9 Females said Methamphetamine (5 were Aboriginal/ 3 were Caucasian/ 1 was Other).
15 Males said Morphine (14 were Aboriginal/ 1 was Caucasian). 13 Males said Fentanyl (9 were Aboriginal/ 4 were Caucasian). 7 Males said Cocaine (2 were Aboriginal/ 5 were Caucasian). 20 Males said Methamphetamine (12 were Aboriginal/ 8 were Caucasian). 3 Males said Heroin (1 was Aboriginal/ 2 were Caucasian).
When conducting our monthly survey, we saw some extreme changes than previous years! Traditionally, we had 50% Morphine users, 32% Crystal Meth users, and 3% Fentanyl users (Cocaine, Heroin, and ADHD medication making up the other 15%). This year, we had 27% Morphine users, 34% Crystal Meth users, and 27% Fentanyl users (Cocaine and Heroin making up the other 12%). Another factor we noticed was our meth pipe distribution has gone up 49.8%, compared to our pipe stats of last year.
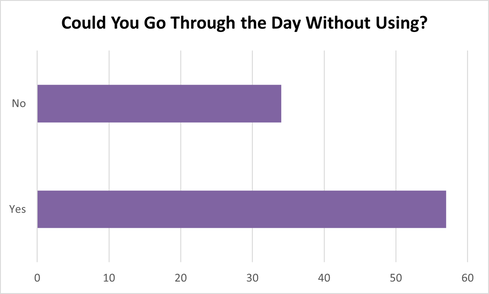
September
21 Females said yes (18 were Aboriginal/ 3 were Caucasian). 13 Females said no (11 were Aboriginal/ 2 were Caucasian).
36 Males said yes (23 were Aboriginal/ 13 were Caucasian). 21 Males said no (14 were Aboriginal/ 5 were Caucasian/ 2 were Other).
Clients expressed that their use increased among certain peers and in certain places. However, many expressed that they could pause for one day if in the right circumstances. One female said that if she were not stressed, she would be able to as she uses substances as a stress reliever.
A quote from a client asked the survey question: “When you’re broke, you sometimes have to (get through the day without using) but that is hard when you’re getting up in age. So, you just pray and thank God for giving you another day.”
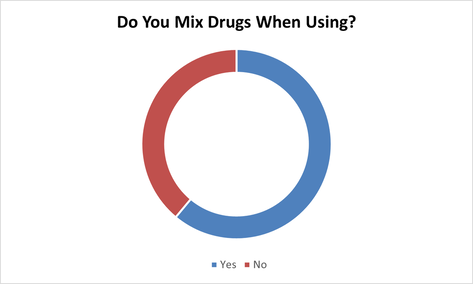
October
17 Females said yes (13 were Aboriginal/ 4 were Caucasian). 10 Females said no (7 were Aboriginal/ 3 were Caucasian).
41 Males said yes (27 were Aboriginal/ 13 were Caucasian/ 1 was Other). 27 Males said no (21 were Aboriginal/ 5 were Caucasian/ 1 was Other).
Client are reporting “Speedballing” (the process of mixing a depressant and a stimulant) with Fentanyl/Crystal Meth and Heroin/Cocaine. Clients were informed that this combination greatly increases the risk of fatal accidental overdose and that Naloxone will work on opioids but in an overdose, 911 needs to be called for stimulant overdoses. When reporting on users who are part of our Naloxone Training Program, Fentanyl and Crystal Meth are the top drugs used followed by Cocaine. In 2020, APSS distributed 2,036 Naloxone kits (averaging 170 kits per month). Of the 2,036 naloxone kits, 985 were used in an overdose situation. Overdoses among our clients, the main drug used is Fentanyl.
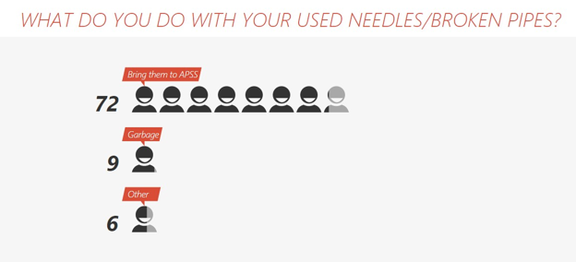
November
24 Females said bring them to APSS (21 were Aboriginal/ 3 were Caucasian). 5 Females said garbage (All were Aboriginal). 3 Females said other (All were Aboriginal).
48 Males said bring to APSS (36 were Aboriginal/ 11 were Caucasian/ 1 was Other). 4 Males said garbage (All were Aboriginal) 3 Males said other (2were Aboriginal/ 1 was Caucasian).
Many told us that they put the equipment in non-pierceable bins before they throw them out, but we explained that bio-hazard equipment such as used syringes need to be disposed of in a specific way. One person told us that they deposit their syringes in the drains. Clients were informed of other sites to drop off used syringes in the city as well as the locations of the yellow disposal bins.
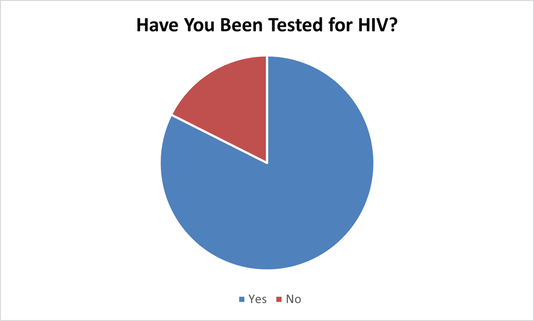
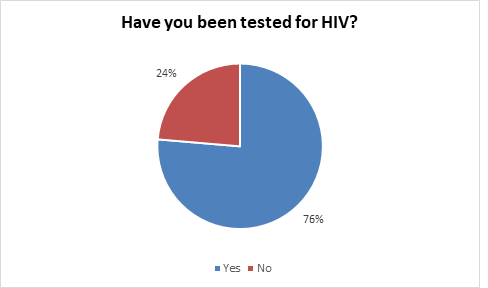
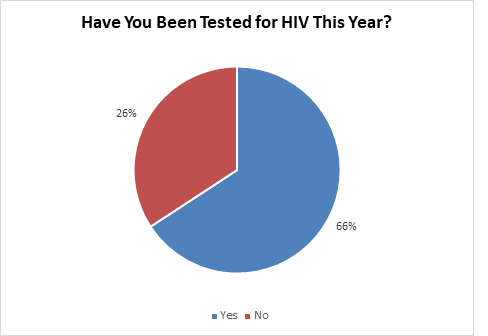
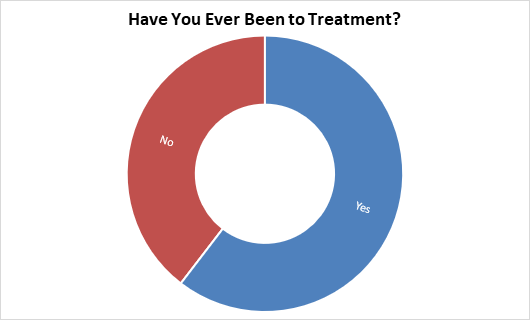
December
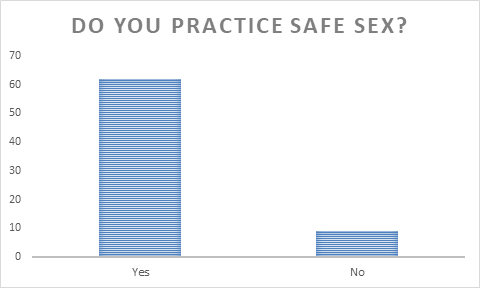
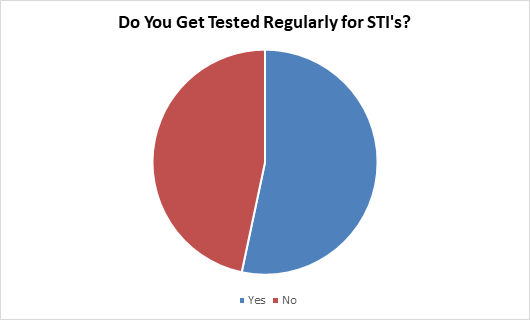
28 Females said yes (22 were Aboriginal/ 6 were Caucasian). 7 Females said no (6 were Aboriginal/ 1 was Caucasian).
47 Males said yes (30 were Aboriginal/ 17 were Caucasian). 9 Males said no (6 were Aboriginal/ 3 were Caucasian).
This year, due to COVID-19, our Thursday testing was halted. Thursday testing will resume once safe to do so.
APSS conducted 10 HCV testing events with local community health professionals and community partner organizations. For events held at our office, a fibro scan was done, and a phlebotomist took blood samples for the lab from mainly an IDU population. A nurse tested through point of care 17 individuals and over 50% were positive for HCV. We were able to get everyone on treatment and connected to care. APSS began working with Four Directions Community Health Centre in October for in-office flu clinics and Coronavirus swab testing every Wednesday. These events are vital for stopping the spread of HCV/COVID-19 in our communities and linking clients to care.