In 2019, we surveyed Needle Exchange clients every month. We asked an anonymous question to different people and then took down their answer and their Needle Exchange ID. This was done to ensure accuracy of results and evade duplicated data. At the end of the three weeks, all data was collected and separated by gender, age, ethnicity, and location. (Graphs were made depending on relevance).
The questions we asked were as followed:
People were very open with their answers, even to the point of going into detail and telling our staff their story. By providing a safe space, being anonymous and having consistent staff, needle exchange clients are more likely to trust us.
The responses from the injection drug users have been informative which have helped in relationship building as well as enhance our programs to meet the needs of our clients. This year, we implemented crack and meth pipes into our exchange after our February survey.
In 2020, we will take this data as a needs assessment and turn what we have learned into where we need to focus. This could include: increased youth education on injection drug use, working with our NEP clients in a way they will understand, and creating awareness events for the public.
The questions we asked were as followed:
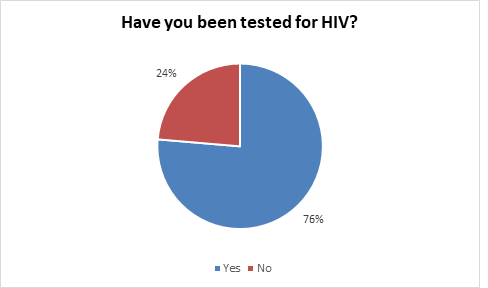
- January- Have you been tested for HIV?
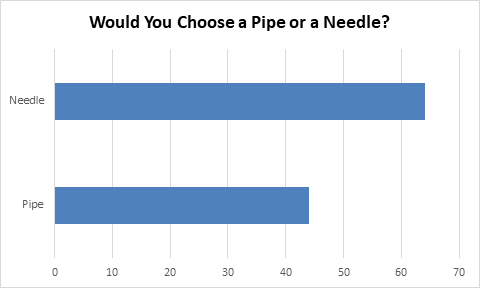
- February- Would you choose a pipe or a needle?
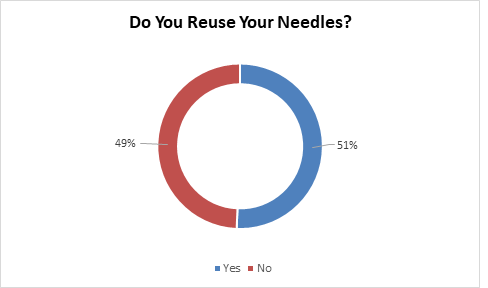
- March- Do you reuse your own needles?
- April- What do you use needles for?
- May- Do you own a Naloxone kit?
- June- How many times do you use a cooker before you use a new one?
- July - When did you start using?
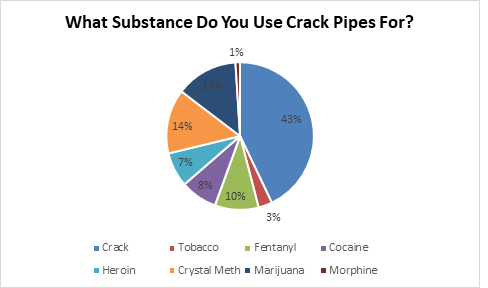
- August- What substance do you use a crack pipe for?
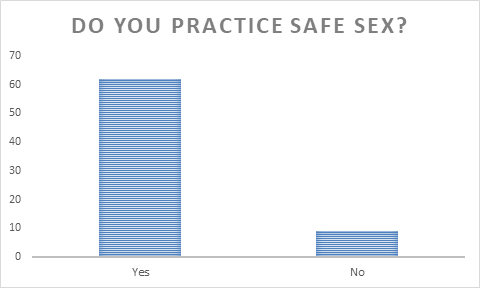
- September- Do you practice safe sex?
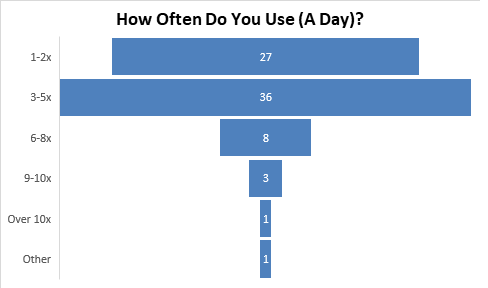
- October- How often do you use a day?
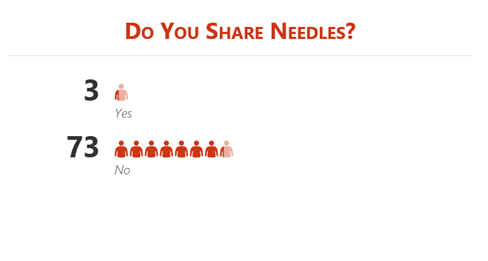
- November- Do you share needles?
- December- Have you been tested for HIV this year?
People were very open with their answers, even to the point of going into detail and telling our staff their story. By providing a safe space, being anonymous and having consistent staff, needle exchange clients are more likely to trust us.
The responses from the injection drug users have been informative which have helped in relationship building as well as enhance our programs to meet the needs of our clients. This year, we implemented crack and meth pipes into our exchange after our February survey.
In 2020, we will take this data as a needs assessment and turn what we have learned into where we need to focus. This could include: increased youth education on injection drug use, working with our NEP clients in a way they will understand, and creating awareness events for the public.
January
8 people asked inquired about getting tested for HIV. One person who said no was informed about our testing, and they got tested that day at our facility. One person said they had not gotten tested for HIV but “knew they had it”. They chose to not get tested because a positive test result would not be able to be ignored.
35 Females said yes (32 were Aboriginal/ 2 were Caucasian/ 1 was Other). 10 Females said no (8 were Aboriginal/ 2 were Caucasian).
36 Males said yes (25 were Aboriginal/ 11 were Caucasian). 12 Males said no (7 were Aboriginal/ 5 were Caucasian).
6 people, in the 3 weeks the survey was being done, were tested for HIV compared to the month of December (4) and the month of November (2). Unfortunately, our nurse is only in on Thursdays for 2 hours which hinders people getting tested.
Testing events were held throughout the year including HIV National Testing Day (June 27th) and AIDS Awareness Week (November 28th). We tested 18 people on June 27th which was the most tested in Regina that day!
In collaboration with health professionals, APSS held four HCV testing events; two of which was held in collaboration with the Newo Yotina Friendship Centre. A nurse tested through point of care 84 individuals. For events held at our office, a fibro scan was done, and a phlebotomist took blood samples for the lab.
35 Females said yes (32 were Aboriginal/ 2 were Caucasian/ 1 was Other). 10 Females said no (8 were Aboriginal/ 2 were Caucasian).
36 Males said yes (25 were Aboriginal/ 11 were Caucasian). 12 Males said no (7 were Aboriginal/ 5 were Caucasian).
6 people, in the 3 weeks the survey was being done, were tested for HIV compared to the month of December (4) and the month of November (2). Unfortunately, our nurse is only in on Thursdays for 2 hours which hinders people getting tested.
Testing events were held throughout the year including HIV National Testing Day (June 27th) and AIDS Awareness Week (November 28th). We tested 18 people on June 27th which was the most tested in Regina that day!
In collaboration with health professionals, APSS held four HCV testing events; two of which was held in collaboration with the Newo Yotina Friendship Centre. A nurse tested through point of care 84 individuals. For events held at our office, a fibro scan was done, and a phlebotomist took blood samples for the lab.
FEBRUARY
6 people answered that it depends on what substance they are using. In our 2018 September monthly survey, “How else do you use drugs besides injecting?”, smoking was the top choice.
Some people were very against pipes saying, “Pipes are hard on the lungs” “Pipes are too dirty”.
15 Females said pipe (14 were Aboriginal/ 1 was Caucasian). 32 Females said needle (28 were Aboriginal/ 3 were Caucasian/ 1 was Other).
29 Males said pipe (26 were Aboriginal/ 3 were Caucasian). 32 Males said needle (27 were Aboriginal/ 5 were Caucasian).
We asked this question before receiving safe inhalation kits (crack/meth pipes) the next month (March 4th) in our needle exchange. We had a huge increase in clients the following months requesting only crack/meth pipes. Currently, we have 376 clients who come to our exchange only for safe inhalation kits.
Clients could receive one crack and meth pipe and were encouraged to bring back the pipes to reduce the number of pipes in the community. We found that clients were not motivated to bring back the pipes as they did not receive an exchange and were using them to the point of shattering.
On October 30th, we began pipe exchange. Our returns increased from 27 to 201.
Some people were very against pipes saying, “Pipes are hard on the lungs” “Pipes are too dirty”.
15 Females said pipe (14 were Aboriginal/ 1 was Caucasian). 32 Females said needle (28 were Aboriginal/ 3 were Caucasian/ 1 was Other).
29 Males said pipe (26 were Aboriginal/ 3 were Caucasian). 32 Males said needle (27 were Aboriginal/ 5 were Caucasian).
We asked this question before receiving safe inhalation kits (crack/meth pipes) the next month (March 4th) in our needle exchange. We had a huge increase in clients the following months requesting only crack/meth pipes. Currently, we have 376 clients who come to our exchange only for safe inhalation kits.
Clients could receive one crack and meth pipe and were encouraged to bring back the pipes to reduce the number of pipes in the community. We found that clients were not motivated to bring back the pipes as they did not receive an exchange and were using them to the point of shattering.
On October 30th, we began pipe exchange. Our returns increased from 27 to 201.
March
5% of people “clean” their needles with bleach before using again. This, however, is not an effective way of cleaning needles for HIV/HCV.
Of the people who said yes, the highest group were in their 30s, followed closely by people in their 20s whereas of the people who said no, the highest group were in their 40s.
20 Females said yes (15 were Aboriginal/ 5 were Caucasian). 14 Females said no (11 were Aboriginal/ 3 were Caucasian).
18 Males said yes (11 were Aboriginal/ 7 were Caucasian). 23 Males said no (18 were Aboriginal/ 5 were Caucasian).
Many clients are knowledgeable on the risks of sharing needles but have coined the phrase “Re-Use Sundays” as no services are open. Many will not share needles with each other but are comfortable re- using their own.
Of the people who said yes, the highest group were in their 30s, followed closely by people in their 20s whereas of the people who said no, the highest group were in their 40s.
20 Females said yes (15 were Aboriginal/ 5 were Caucasian). 14 Females said no (11 were Aboriginal/ 3 were Caucasian).
18 Males said yes (11 were Aboriginal/ 7 were Caucasian). 23 Males said no (18 were Aboriginal/ 5 were Caucasian).
Many clients are knowledgeable on the risks of sharing needles but have coined the phrase “Re-Use Sundays” as no services are open. Many will not share needles with each other but are comfortable re- using their own.
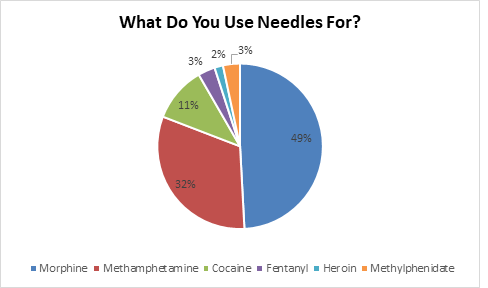
April
28.8% of all people who said morphine specified that they did hydromorphone, which is approximately 5 times stronger than morphine.
23 Females said Morphine (19 were Aboriginal/ 4 were Caucasian). 16 Female said Methamphetamine (14 were Aboriginal/ 2 were Caucasian). 7 Females said Cocaine (6 were Aboriginal/ 1 was Caucasian). 2 Females said Methylphenidate (Both are Aboriginal).
37 Males said Morphine (32 were Aboriginal/ 5 were Caucasian). 22 Males said Methamphetamine (18 were Aboriginal/ 4 were Caucasian). 5 Males said Cocaine (3 were Aboriginal/ 2 were Caucasian). 4 Males said Fentanyl (3 were Aboriginal/ 1 was Caucasian). 2 Males said Heroin (Both are Caucasian). 2 Males said Methylphenidate (Both are Aboriginal).
Listed on the graph are the medical drug names but in the Needle exchange we received the following drug slang: Down, Side, Sets, T’s and R’s, Coke, Up, and Jib.
As Crystal Meth use rises in Regina, we are still seeing a constant in Morphine use in our clients. However, from our last years surveys, meth use increased by over double from 7 (2017) to 16 (2018) to 39 (2019). However, the amount of meth pipes given out in our exchange daily is high, and this question was asked specifically for needle use.
23 Females said Morphine (19 were Aboriginal/ 4 were Caucasian). 16 Female said Methamphetamine (14 were Aboriginal/ 2 were Caucasian). 7 Females said Cocaine (6 were Aboriginal/ 1 was Caucasian). 2 Females said Methylphenidate (Both are Aboriginal).
37 Males said Morphine (32 were Aboriginal/ 5 were Caucasian). 22 Males said Methamphetamine (18 were Aboriginal/ 4 were Caucasian). 5 Males said Cocaine (3 were Aboriginal/ 2 were Caucasian). 4 Males said Fentanyl (3 were Aboriginal/ 1 was Caucasian). 2 Males said Heroin (Both are Caucasian). 2 Males said Methylphenidate (Both are Aboriginal).
Listed on the graph are the medical drug names but in the Needle exchange we received the following drug slang: Down, Side, Sets, T’s and R’s, Coke, Up, and Jib.
As Crystal Meth use rises in Regina, we are still seeing a constant in Morphine use in our clients. However, from our last years surveys, meth use increased by over double from 7 (2017) to 16 (2018) to 39 (2019). However, the amount of meth pipes given out in our exchange daily is high, and this question was asked specifically for needle use.
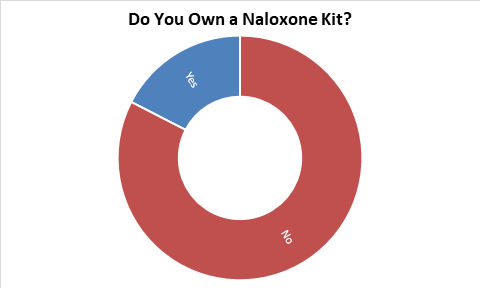
May
12 people inquired about getting training. One person was upset to hear that we offer free kits to anyone trained as she had been purchasing them off the street for an inflated price.
3 Females said yes (2 were Aboriginal/ 1 was Caucasian). 36 Females said no (27 were Aboriginal/ 9 were Caucasian).
12 Males said yes (8 were Aboriginal/ 4 were Caucasian). 35 Males said no (25 were Aboriginal/ 10 was Caucasian).
With the high levels of interest in Naloxone kits and training, APSS became a distribution site in November 2018. All APSS staff have been trained and will be able to train anyone interested in Naloxone. The training, depending on those being trained, takes 15 minutes and trains individuals on how to administer the drug, how to identify an overdose, and overdose prevention. In 2019, we trained 206 people and replaced 84 kits that were used in an overdose (gave out 353 kits).
One person had just lost a friend to an overdose the day before.
In a separate overdose survey, 66% of people surveyed have overdosed. Of people surveyed, 50% have witnessed 1-5 overdoes and 33.3% have witnessed over 15 overdoses. 1 person answered that they have never witnessed an overdose. When asked if they knew someone who had died from an overdose, our most chosen answer was over 5 people.
3 Females said yes (2 were Aboriginal/ 1 was Caucasian). 36 Females said no (27 were Aboriginal/ 9 were Caucasian).
12 Males said yes (8 were Aboriginal/ 4 were Caucasian). 35 Males said no (25 were Aboriginal/ 10 was Caucasian).
With the high levels of interest in Naloxone kits and training, APSS became a distribution site in November 2018. All APSS staff have been trained and will be able to train anyone interested in Naloxone. The training, depending on those being trained, takes 15 minutes and trains individuals on how to administer the drug, how to identify an overdose, and overdose prevention. In 2019, we trained 206 people and replaced 84 kits that were used in an overdose (gave out 353 kits).
One person had just lost a friend to an overdose the day before.
In a separate overdose survey, 66% of people surveyed have overdosed. Of people surveyed, 50% have witnessed 1-5 overdoes and 33.3% have witnessed over 15 overdoses. 1 person answered that they have never witnessed an overdose. When asked if they knew someone who had died from an overdose, our most chosen answer was over 5 people.
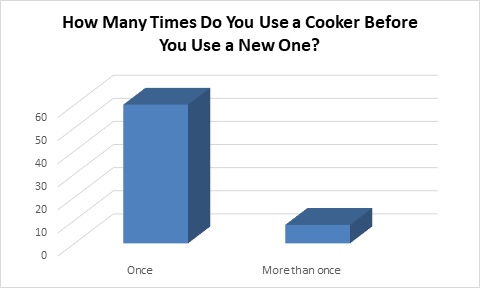
June
88% of people asked knew that cookers can only be used one as the supplies we have rust. We also let our clients know that studies have now released that HIV can be transmitted through cookers and other drug equipment.
23 Females said once (22 were Aboriginal/ 1 was Caucasian). 6 Females said more than once (4 were Aboriginal/ 2 were Caucasian)
37 Males said once (28 were Aboriginal/ 9 was Caucasian). 2 Males said more than once (1 was Aboriginal/ 1 was Caucasian).
One person specified that they use a new cooker per new pill which depending on the pill, will depend on the amount of hits. A few people mentioned that they find cookers dirty and prefer to use spoons.
23 Females said once (22 were Aboriginal/ 1 was Caucasian). 6 Females said more than once (4 were Aboriginal/ 2 were Caucasian)
37 Males said once (28 were Aboriginal/ 9 was Caucasian). 2 Males said more than once (1 was Aboriginal/ 1 was Caucasian).
One person specified that they use a new cooker per new pill which depending on the pill, will depend on the amount of hits. A few people mentioned that they find cookers dirty and prefer to use spoons.
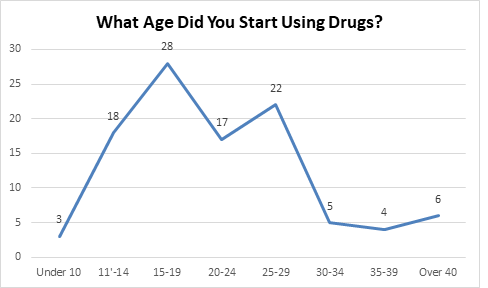
July
39% of people who said they started between the ages of 15-19, started at 18; 18% started at 16. This was only for injection drugs, meaning they could have started smoking (tobacco or marijuana) or drinking alcohol much earlier. Three people specified that they started smoking marijuana at 11/12 but started injection drugs much later in life.
1 Female said under 10 years old (She was Aboriginal). 10 Females said 11-14 years old (9 were Aboriginal/1 was Caucasian). 12 Females said 15-19 years old (11 were Aboriginal/ 1 was Caucasian). 9 Females said 20-24 years old (All were Aboriginal). 13 Females said 25-29 years old (All were Aboriginal). 1 Female said 30-34 years old (She was Aboriginal). 1 Female said 35-39 years old (She was Aboriginal). 2 Females said over 40 years old (They were Aboriginal).
2 Males said under 10 years old (They were Aboriginal). 8 Males said 11-14 years old (6 were Aboriginal/2 were Caucasian). 16 Males said 15-19 years old (13 were Aboriginal/ 3 were Caucasian). 8 Males said 20-24 years old (6 were Aboriginal/2 were Caucasian). 9 Males said 25-29 years old (5 were Aboriginal/ 4 were Caucasian). 4 Males said 30-34 years old (2 were Aboriginal/ 1 was Caucasian/ 1 was Other). 3 Males said 35-39 years old (All were Aboriginal). 4 Males said over 40 years old (All were Aboriginal).
Our youngest answer for injecting drugs was 7 years old and this year we saw an increase in younger users who started using drugs from 11-14 years old from 10 (2018) to 18 (2019).
1 Female said under 10 years old (She was Aboriginal). 10 Females said 11-14 years old (9 were Aboriginal/1 was Caucasian). 12 Females said 15-19 years old (11 were Aboriginal/ 1 was Caucasian). 9 Females said 20-24 years old (All were Aboriginal). 13 Females said 25-29 years old (All were Aboriginal). 1 Female said 30-34 years old (She was Aboriginal). 1 Female said 35-39 years old (She was Aboriginal). 2 Females said over 40 years old (They were Aboriginal).
2 Males said under 10 years old (They were Aboriginal). 8 Males said 11-14 years old (6 were Aboriginal/2 were Caucasian). 16 Males said 15-19 years old (13 were Aboriginal/ 3 were Caucasian). 8 Males said 20-24 years old (6 were Aboriginal/2 were Caucasian). 9 Males said 25-29 years old (5 were Aboriginal/ 4 were Caucasian). 4 Males said 30-34 years old (2 were Aboriginal/ 1 was Caucasian/ 1 was Other). 3 Males said 35-39 years old (All were Aboriginal). 4 Males said over 40 years old (All were Aboriginal).
Our youngest answer for injecting drugs was 7 years old and this year we saw an increase in younger users who started using drugs from 11-14 years old from 10 (2018) to 18 (2019).
August
34.5% of people who answered Crystal Meth specified that they use it for “hot rails” (the act of snorting a line of crystal meth through the nose by heating up the end of a glass pipe and then opening your mouth to release white smoke).
39 Females said Crack (35 were Aboriginal/ 4 were Caucasian). 3 Females said Tobacco (All were Aboriginal). 9 Females said Fentanyl (7 were Aboriginal/ 2 were Caucasian). 8 Females said Cocaine (All were Aboriginal). 8 Females said Heroin (7 were Aboriginal/ 1 was Caucasian). 10 Females said Crystal Meth (All were Aboriginal). 8 Females said Marijuana (7 were Aboriginal/ 1 was Caucasian).
46 Males said Crack (34 were Aboriginal/ 11 were Caucasian/ 1 was Other). 3 Males said tobacco (All were Aboriginal). 10 Males said Fentanyl (6 were Aboriginal/ 4 were Caucasian). 8 Males said Cocaine (4 were Aboriginal/ 4 were Caucasian). 7 Males said Heroin (3 were Aboriginal/ 4 were Caucasian). 18 Males said Crystal Meth (13 were Aboriginal/ 5 was Caucasian). 19 Males said Marijuana (12 were Aboriginal/ 7 were Caucasian). 2 Males said Morphine (both were Aboriginal).
When we were working out how the pipes were to be distributed, clients would take both pipes as they could only get one of each pipe per day, even though some only use meth. People told us they would either sell the crack pipe ($10), keep it in case anyone using with them needed it, or use it to smoke meth.
One client even said they make a makeshift meth pipe from the crack pipe for “meth when my meth pipe is done.”. We also had many people comment that they were using the “straight” pipes as a weed/tobacco pipe since legalization of Marijuana in Canada last October.
39 Females said Crack (35 were Aboriginal/ 4 were Caucasian). 3 Females said Tobacco (All were Aboriginal). 9 Females said Fentanyl (7 were Aboriginal/ 2 were Caucasian). 8 Females said Cocaine (All were Aboriginal). 8 Females said Heroin (7 were Aboriginal/ 1 was Caucasian). 10 Females said Crystal Meth (All were Aboriginal). 8 Females said Marijuana (7 were Aboriginal/ 1 was Caucasian).
46 Males said Crack (34 were Aboriginal/ 11 were Caucasian/ 1 was Other). 3 Males said tobacco (All were Aboriginal). 10 Males said Fentanyl (6 were Aboriginal/ 4 were Caucasian). 8 Males said Cocaine (4 were Aboriginal/ 4 were Caucasian). 7 Males said Heroin (3 were Aboriginal/ 4 were Caucasian). 18 Males said Crystal Meth (13 were Aboriginal/ 5 was Caucasian). 19 Males said Marijuana (12 were Aboriginal/ 7 were Caucasian). 2 Males said Morphine (both were Aboriginal).
When we were working out how the pipes were to be distributed, clients would take both pipes as they could only get one of each pipe per day, even though some only use meth. People told us they would either sell the crack pipe ($10), keep it in case anyone using with them needed it, or use it to smoke meth.
One client even said they make a makeshift meth pipe from the crack pipe for “meth when my meth pipe is done.”. We also had many people comment that they were using the “straight” pipes as a weed/tobacco pipe since legalization of Marijuana in Canada last October.
September
33.3% of all people who said no said they were married/ only with one partner.
3 women self-identified as street workers and all of them said they practice safe sex by using condoms, dental dams, and lube.
30 Females said yes (24 were Aboriginal/ 6 were Caucasian). 4 Females said no (3 were Aboriginal/ 1 was Caucasian).
32 Males said yes (28 were Aboriginal/ 4 were Caucasian). 5 Males said no (2 were Aboriginal/ 3 were Caucasian).
In 2019, we gave out 25,630 condoms in our needle exchange program.
3 women self-identified as street workers and all of them said they practice safe sex by using condoms, dental dams, and lube.
30 Females said yes (24 were Aboriginal/ 6 were Caucasian). 4 Females said no (3 were Aboriginal/ 1 was Caucasian).
32 Males said yes (28 were Aboriginal/ 4 were Caucasian). 5 Males said no (2 were Aboriginal/ 3 were Caucasian).
In 2019, we gave out 25,630 condoms in our needle exchange program.
October
The “Other” category included a value that did not fit in our time frame (once a week).
55.5% of all people who fell in the 3-5x category, said they used 3 times a day and even went into detail to say they use when they wake up, halfway through the day, and at night.
10 Females said 1-2x (9 were Aboriginal/ 1 was Caucasian). 14 Females said 3-5x (13 were Aboriginal/1 was Caucasian). 3 Females said 6-8x (2 were Aboriginal/ 1 was Caucasian). 1 Female said 9-10x (She was Caucasian).
17 Males said 1-2x (15 were Aboriginal/ 2 were Caucasian). 22 Males said 3-5x (15 were Aboriginal/ 7 were Caucasian). 5 Males said 6-8x (3 were Aboriginal/ 1 was Caucasian/ 1 was Other). 2 Males said 9-10x (1 was Aboriginal/ 1 was Caucasian). 1 Male said over 10x (He was Aboriginal). 1 Male said other (He was Aboriginal).
The person who was using 20x a day, did not specify what drug they use but, use small amounts of drug many times. A woman told us that she used to use 15x a day but wants to quit and has lowered her use to 2-3 times a day. Many answered specific numbers of use however one man told us he uses twice a day minimum.
55.5% of all people who fell in the 3-5x category, said they used 3 times a day and even went into detail to say they use when they wake up, halfway through the day, and at night.
10 Females said 1-2x (9 were Aboriginal/ 1 was Caucasian). 14 Females said 3-5x (13 were Aboriginal/1 was Caucasian). 3 Females said 6-8x (2 were Aboriginal/ 1 was Caucasian). 1 Female said 9-10x (She was Caucasian).
17 Males said 1-2x (15 were Aboriginal/ 2 were Caucasian). 22 Males said 3-5x (15 were Aboriginal/ 7 were Caucasian). 5 Males said 6-8x (3 were Aboriginal/ 1 was Caucasian/ 1 was Other). 2 Males said 9-10x (1 was Aboriginal/ 1 was Caucasian). 1 Male said over 10x (He was Aboriginal). 1 Male said other (He was Aboriginal).
The person who was using 20x a day, did not specify what drug they use but, use small amounts of drug many times. A woman told us that she used to use 15x a day but wants to quit and has lowered her use to 2-3 times a day. Many answered specific numbers of use however one man told us he uses twice a day minimum.
November
Of all people asked, 3 (all men) expressed that they share needles, however, each specified their answer with “sometimes” “I try not too” and “only with my wife”.
28 Females said no (24 were Aboriginal/ 4 were Caucasian).
3 Males said yes (1 were Aboriginal/ 2 was Caucasian). 45 Males said no (34 were Aboriginal/ 10 were Caucasian/ 1 was Other).
Back in March, we asked if clients reuse their own needles and they were more open to reusing their own needles vs. sharing with others when services are not available (“Re-use Sundays”).
We continue to educate our clients in the needle exchange with quick informative tips and handbills. Information includes harm reduction such as overdose prevention, HIV information on down to reduce the spread of HIV, STI information and where to get tested, and addiction information for treatment. This year, 2,679 conversations were made with 1,215 in relation to harm reduction.
28 Females said no (24 were Aboriginal/ 4 were Caucasian).
3 Males said yes (1 were Aboriginal/ 2 was Caucasian). 45 Males said no (34 were Aboriginal/ 10 were Caucasian/ 1 was Other).
Back in March, we asked if clients reuse their own needles and they were more open to reusing their own needles vs. sharing with others when services are not available (“Re-use Sundays”).
We continue to educate our clients in the needle exchange with quick informative tips and handbills. Information includes harm reduction such as overdose prevention, HIV information on down to reduce the spread of HIV, STI information and where to get tested, and addiction information for treatment. This year, 2,679 conversations were made with 1,215 in relation to harm reduction.
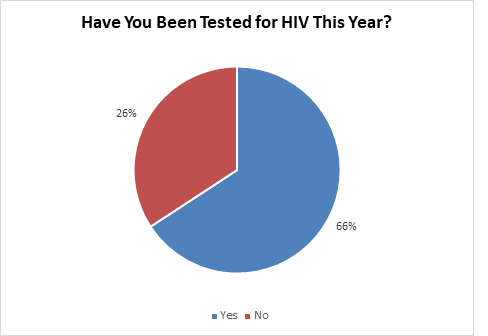
December
2 people, in the 3 weeks the survey was being done, were tested for HIV compared to the month of October (4) and the month of November (4). Unfortunately, our nurse is only in on Thursdays for 2 hours which hinders people getting tested.
18 Females said yes (17 were Aboriginal/1 was Caucasian). 10 Females said no (7 were Aboriginal/ 3 were Caucasian).
32 Males said yes (25 were Aboriginal/7 were Caucasian). 16 Males said no (11 were Aboriginal/ 4 were Caucasian/1 was Other).
When comparing our results from January, we found that many clients have been tested for HIV but do not keep up with yearly tests. Many chose to get tested at the beginning of the year vs. at the end of the year (Tested 6 in January for HIV; 2 in December).
While asking the question, 149 HIV conversations were had on why to get tested, how the test works, and where to get tested.
18 Females said yes (17 were Aboriginal/1 was Caucasian). 10 Females said no (7 were Aboriginal/ 3 were Caucasian).
32 Males said yes (25 were Aboriginal/7 were Caucasian). 16 Males said no (11 were Aboriginal/ 4 were Caucasian/1 was Other).
When comparing our results from January, we found that many clients have been tested for HIV but do not keep up with yearly tests. Many chose to get tested at the beginning of the year vs. at the end of the year (Tested 6 in January for HIV; 2 in December).
While asking the question, 149 HIV conversations were had on why to get tested, how the test works, and where to get tested.