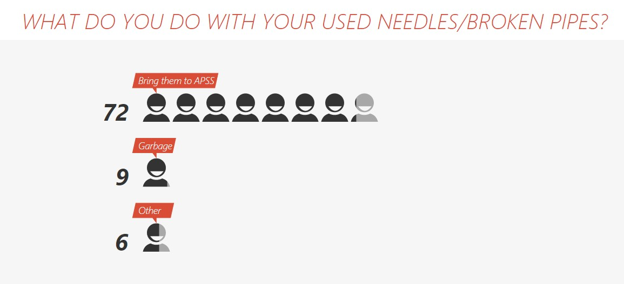
In 2017, we surveyed Needle Exchange clients for 3 weeks every month. We asked an anonymous question to 120 different people and then took down their answer and their Needle Exchange ID. This was done to ensure accuracy of results and evade duplicated data. At the end of the three weeks, all data was collected and separated by gender, age, ethnicity, and location. (Graphs were made depending on relevance).
The questions we asked were as followed:
People were very open with their answers, even to the point of going into detail and telling our staff their story. By providing a safe space, being anonymous and having consistent staff, needle exchange clients are more likely to trust us.
From our everyday stats, only 16% of people picking up needles are Caucasian. We make sure to keep that percentage with everyone we ask.
The responses from the injection drug users have been informative which have helped in relationship building as well as enhance our programs to meet the needs of our clients.
In 2018, we will take this data as a needs assessment and turn what we have learned into where we need to focus. This could include: increased youth education on injection drug use, working with our NEP clients in a way they will understand, and creating awareness events for the public.
The questions we asked were as followed:
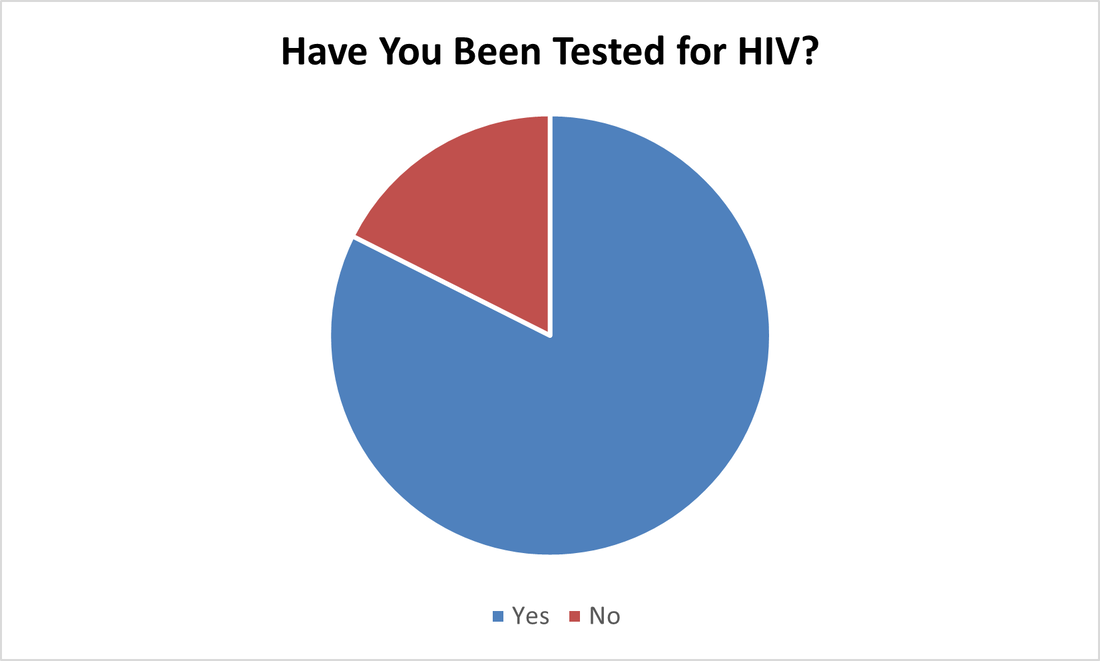
- January- Have you been tested for HIV?
- February- Do you use protection?
- March- What do you use needles for? (What drug?)
- April- How often do you use a day?
- May- What was your first drug? (Alcohol/Nicotine/Marijuana/Other)
- June- Have you ever been to treatment? (Substance/alcohol)
- July- When did you start using?
- August- Why did you start using?
- September- Do people know you use?
- October- Have you ever overdosed?
- November- Have you ever been refused services or felt stigmatized because of your use?
- December- Have you been tested for HIV this year? (a repeat question to compare results from January)
People were very open with their answers, even to the point of going into detail and telling our staff their story. By providing a safe space, being anonymous and having consistent staff, needle exchange clients are more likely to trust us.
From our everyday stats, only 16% of people picking up needles are Caucasian. We make sure to keep that percentage with everyone we ask.
The responses from the injection drug users have been informative which have helped in relationship building as well as enhance our programs to meet the needs of our clients.
In 2018, we will take this data as a needs assessment and turn what we have learned into where we need to focus. This could include: increased youth education on injection drug use, working with our NEP clients in a way they will understand, and creating awareness events for the public.
January
10.8% of all people asked, inquired about testing (8 of the 13 were Female)
53 Females said yes (49 were Aboriginal/ 4 were Caucasian). 8 Females said no (7 were Aboriginal/ 1 was Caucasian)
50 Males said yes (37 were Aboriginal/ 12 were Caucasian/ 1 was Other). 9 Males said no (7 were Aboriginal/ 2 were Caucasian)
9 people, in the 3 weeks the survey was being done, were tested for HIV compared to the month of December (1) and the month of November (7). Unfortunately, our nurse is only in on Thursdays for 2 hours which hinders people getting tested.
When asked, a few prompted to say that they regularly get tested due to the high risk activities they indulge in.
53 Females said yes (49 were Aboriginal/ 4 were Caucasian). 8 Females said no (7 were Aboriginal/ 1 was Caucasian)
50 Males said yes (37 were Aboriginal/ 12 were Caucasian/ 1 was Other). 9 Males said no (7 were Aboriginal/ 2 were Caucasian)
9 people, in the 3 weeks the survey was being done, were tested for HIV compared to the month of December (1) and the month of November (7). Unfortunately, our nurse is only in on Thursdays for 2 hours which hinders people getting tested.
When asked, a few prompted to say that they regularly get tested due to the high risk activities they indulge in.
FEBRUARY
45.5% of all people who said no said they were married/ only with one partner.
37 Females said yes (32 were Aboriginal/ 5 were Caucasian). 20 Females said no (18 were Aboriginal/ 1 was Caucasian/ 1 was Other). 2 Females said sometimes (1 was Aboriginal/ 1 was Caucasian)
46 Males said yes (39 were Aboriginal/ 7 were Caucasian). 13 Males said no (11 were Aboriginal/ 2 were Caucasian). 2 Males said sometimes (Both were Aboriginal)
The answers for people surveyed under the age of 24 (1993) were all yes to using protection except for 1 who self-identified as lesbian.
We can take from this that sexual education in schools is doing a great job.
37 Females said yes (32 were Aboriginal/ 5 were Caucasian). 20 Females said no (18 were Aboriginal/ 1 was Caucasian/ 1 was Other). 2 Females said sometimes (1 was Aboriginal/ 1 was Caucasian)
46 Males said yes (39 were Aboriginal/ 7 were Caucasian). 13 Males said no (11 were Aboriginal/ 2 were Caucasian). 2 Males said sometimes (Both were Aboriginal)
The answers for people surveyed under the age of 24 (1993) were all yes to using protection except for 1 who self-identified as lesbian.
We can take from this that sexual education in schools is doing a great job.
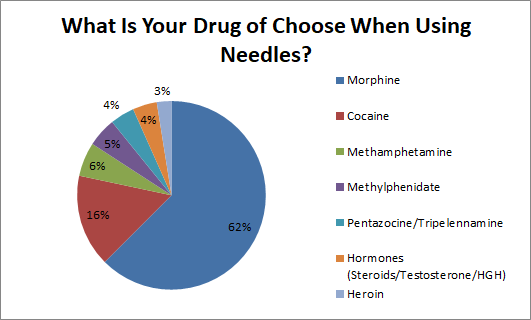
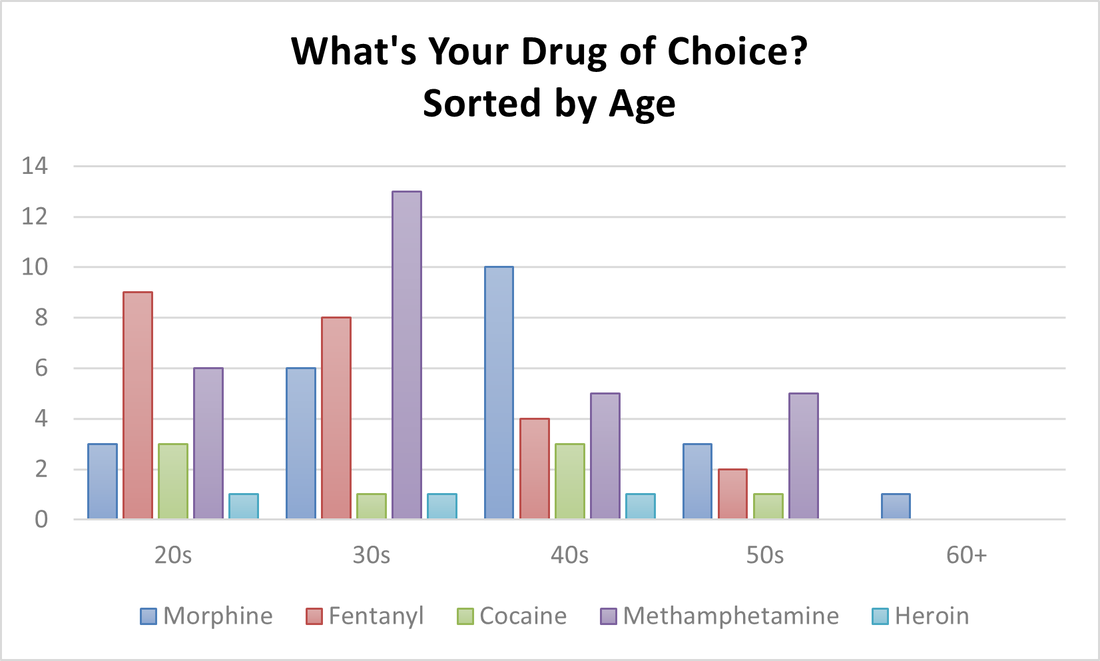
March
10.6% of all people who said morphine specified that they did Hydromorphone, which is approximately 5 times stronger than Morphine.
32 Females said Morphine (28 were Aboriginal/ 3 were Caucasian/ 1 was Other). 11 Females said cocaine (8 were Aboriginal/ 3 were Caucasian). 1 Female said Methamphetamine (She was Caucasian). 3 Females said Methylphenidate (All were Aboriginal). 3 Females said Pentazocine/ Pripelennamine (All were Aboriginal). 1 Female said Heroin (She was Caucasian).
43 Males said Morphine (38 were Aboriginal/ 5 were Caucasian). 8 Males said Cocaine (6 were Aboriginal/ 1 was Caucasian/ 1 was Other). 6 Males said Methamphetamines (5 were Aboriginal/ 1 was Caucasian). 3 Males said Methylphenidate (All were Aboriginal). 2 Males said Pentazocine/ Tripelennamine (1 was Aboriginal/1 was Caucasian). 5 Males said Hormones (1 was Aboriginal/ 4 were Caucasian). 2 Males said Heroin (1 was Aboriginal/ 1 was Caucasian).
Listed on the graph are the medical drug names but in the Needle exchange we received the following drug slang: Down, Side, Sets, T’s and R’s, Coke, Up, and Jib.
With the rise of Fentanyl in Regina, 2 males identified that they use it as well as their main drug, but one stopped using it after almost overdosing.
32 Females said Morphine (28 were Aboriginal/ 3 were Caucasian/ 1 was Other). 11 Females said cocaine (8 were Aboriginal/ 3 were Caucasian). 1 Female said Methamphetamine (She was Caucasian). 3 Females said Methylphenidate (All were Aboriginal). 3 Females said Pentazocine/ Pripelennamine (All were Aboriginal). 1 Female said Heroin (She was Caucasian).
43 Males said Morphine (38 were Aboriginal/ 5 were Caucasian). 8 Males said Cocaine (6 were Aboriginal/ 1 was Caucasian/ 1 was Other). 6 Males said Methamphetamines (5 were Aboriginal/ 1 was Caucasian). 3 Males said Methylphenidate (All were Aboriginal). 2 Males said Pentazocine/ Tripelennamine (1 was Aboriginal/1 was Caucasian). 5 Males said Hormones (1 was Aboriginal/ 4 were Caucasian). 2 Males said Heroin (1 was Aboriginal/ 1 was Caucasian).
Listed on the graph are the medical drug names but in the Needle exchange we received the following drug slang: Down, Side, Sets, T’s and R’s, Coke, Up, and Jib.
With the rise of Fentanyl in Regina, 2 males identified that they use it as well as their main drug, but one stopped using it after almost overdosing.
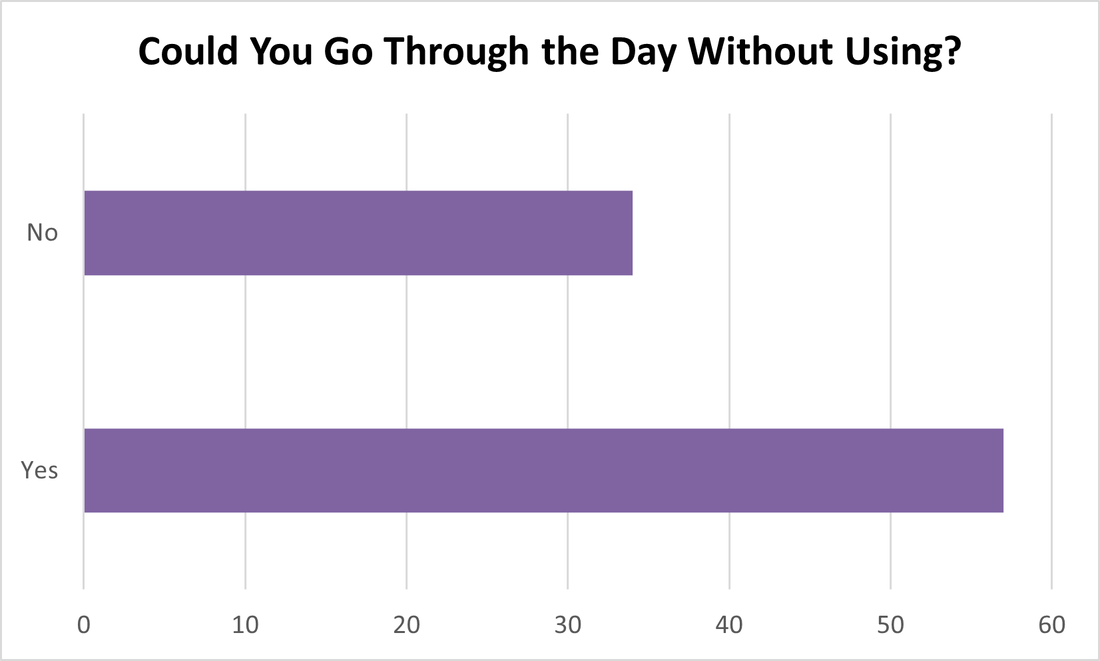
April
The “Other” category included values that did not fit in our time frame such as 2x a month, 1x every few days, and 2x a week.
43.6% of all people who fell in the 3-5x category, said they used 4 times a day and even went into detail to say they did it once in the morning, once in the afternoon, once around supper time, and once at night.
19 Females said 1-2x (16 were Aboriginal/ 2 were Caucasian/ 1 was Other). 22 Females said 3-5x (21 were Aboriginal/1 was Caucasian). 2 Females said 6-8x (both were Aboriginal). 1 Female said 9-10x (she was Aboriginal). 3 Females said over 10x (2 were Aboriginal/ 1 was Caucasian). 3 Females said other (all were Aboriginal).
18 Males said 1-2x (13 were Aboriginal/ 4 were Caucasian/ 1 was Other). 33 Males said 3-5x (29 were Aboriginal/ 4 were Caucasian). 8 Males said 6-8x (6 were Aboriginal/ 2 were Caucasian). 6 Males said 9-10x (3 were Aboriginal/ 3 were Caucasian). 2 Males said over 10x (both were Aboriginal). 3 Males said other (all were Aboriginal).
Spikes in use a day (10x or over) included a man who had just been cut off methadone, a woman who was using 20x a day (small hits) after her recent relapse, and a man who answered the question with “Well, I spend $100 a day on drugs so…”.
When asking such a question, it can trigger emotions. When asked, a man broke down and cried. He was using 3x a day but he wanted to quit. We were able to refer him to different services to aid his recovery, but he admitted he was not ready for treatment. He would, however, return when he was ready.
43.6% of all people who fell in the 3-5x category, said they used 4 times a day and even went into detail to say they did it once in the morning, once in the afternoon, once around supper time, and once at night.
19 Females said 1-2x (16 were Aboriginal/ 2 were Caucasian/ 1 was Other). 22 Females said 3-5x (21 were Aboriginal/1 was Caucasian). 2 Females said 6-8x (both were Aboriginal). 1 Female said 9-10x (she was Aboriginal). 3 Females said over 10x (2 were Aboriginal/ 1 was Caucasian). 3 Females said other (all were Aboriginal).
18 Males said 1-2x (13 were Aboriginal/ 4 were Caucasian/ 1 was Other). 33 Males said 3-5x (29 were Aboriginal/ 4 were Caucasian). 8 Males said 6-8x (6 were Aboriginal/ 2 were Caucasian). 6 Males said 9-10x (3 were Aboriginal/ 3 were Caucasian). 2 Males said over 10x (both were Aboriginal). 3 Males said other (all were Aboriginal).
Spikes in use a day (10x or over) included a man who had just been cut off methadone, a woman who was using 20x a day (small hits) after her recent relapse, and a man who answered the question with “Well, I spend $100 a day on drugs so…”.
When asking such a question, it can trigger emotions. When asked, a man broke down and cried. He was using 3x a day but he wanted to quit. We were able to refer him to different services to aid his recovery, but he admitted he was not ready for treatment. He would, however, return when he was ready.
May
Attending a recent training, we were approached by someone who asked if marijuana is a gateway drug. The definition of a gateway drug is a habit-forming drug that, while not itself addictive, may lead to the use of other addictive drugs.
The “Other” category included any drug that did not fit in the other categories. 43.5% were prescription drugs and 47.8% were hard drugs like cocaine and morphine.
12 Females said alcohol (9 were Aboriginal/ 3 were Caucasian). 18 Females said marijuana (16 were Aboriginal/ 2 were Caucasian). 18 Females said nicotine (12 were Aboriginal/ 6 were Caucasian). 13 Female said other (All were Aboriginal).
18 Males said alcohol (13 were Aboriginal/ 5 were Caucasian). 25 Males said marijuana (20 were Aboriginal/ 5 were Caucasian). 6 Males said nicotine (5 were Aboriginal/ 1 was Caucasian). 10 Male said other (7 were Aboriginal/ 3 were Caucasian).
One woman said alcohol was the gateway drug due to its easy availability and terrible withdrawal symptoms.
Perhaps our results show that marijuana is a “gateway drug” but many who were asked the survey question did not view nicotine or alcohol as a drug even though the definition of a drug is “a substance which has a physiological effect when ingested or otherwise introduced into the body”.
The “Other” category included any drug that did not fit in the other categories. 43.5% were prescription drugs and 47.8% were hard drugs like cocaine and morphine.
12 Females said alcohol (9 were Aboriginal/ 3 were Caucasian). 18 Females said marijuana (16 were Aboriginal/ 2 were Caucasian). 18 Females said nicotine (12 were Aboriginal/ 6 were Caucasian). 13 Female said other (All were Aboriginal).
18 Males said alcohol (13 were Aboriginal/ 5 were Caucasian). 25 Males said marijuana (20 were Aboriginal/ 5 were Caucasian). 6 Males said nicotine (5 were Aboriginal/ 1 was Caucasian). 10 Male said other (7 were Aboriginal/ 3 were Caucasian).
One woman said alcohol was the gateway drug due to its easy availability and terrible withdrawal symptoms.
Perhaps our results show that marijuana is a “gateway drug” but many who were asked the survey question did not view nicotine or alcohol as a drug even though the definition of a drug is “a substance which has a physiological effect when ingested or otherwise introduced into the body”.
June
11% of people who said no, inquired about treatment options. One person who had already been to treatment asked about other treatment options. We asked if people had chosen to go to treatment or were referred. This could include court referred, doctor referred and interventions between family and friends.
33 Females said yes (27were Aboriginal/ 6 were Caucasian/). 16 Females said no (13 were Aboriginal/ 3 were Caucasian).
11 Females said they were referred (9 were Aboriginal/ 2 were Caucasian). 22 Females said it was their choice (18 were Aboriginal/ 4 were Caucasian).
50 Males said yes (35 were Aboriginal/ 14 were Caucasian/ 1 was Other). 21 Males said no (18 were Aboriginal/ 3 were Caucasian).
15 Males said they were referred (9 were Aboriginal/ 6 were Caucasian). 35 Males said it was their choice (26 were Aboriginal/ 8 were Caucasian/ 1 was Other).
With such high rates of people saying they had gone to treatment but were still dealing with addictions, we conducted a second survey asking if treatment works.
2 of the 20 people asked said no. One even went as far to say that talking about treatment, made her want to do drugs more. The other 18 said that treatment works as long as you are in the right mindset. One man said that he enjoyed going to treatment, as it was a kind of “holiday” where he only had to concentrate on himself. The only problem was when he returned home, he fell back into the addiction cycle.
33 Females said yes (27were Aboriginal/ 6 were Caucasian/). 16 Females said no (13 were Aboriginal/ 3 were Caucasian).
11 Females said they were referred (9 were Aboriginal/ 2 were Caucasian). 22 Females said it was their choice (18 were Aboriginal/ 4 were Caucasian).
50 Males said yes (35 were Aboriginal/ 14 were Caucasian/ 1 was Other). 21 Males said no (18 were Aboriginal/ 3 were Caucasian).
15 Males said they were referred (9 were Aboriginal/ 6 were Caucasian). 35 Males said it was their choice (26 were Aboriginal/ 8 were Caucasian/ 1 was Other).
With such high rates of people saying they had gone to treatment but were still dealing with addictions, we conducted a second survey asking if treatment works.
2 of the 20 people asked said no. One even went as far to say that talking about treatment, made her want to do drugs more. The other 18 said that treatment works as long as you are in the right mindset. One man said that he enjoyed going to treatment, as it was a kind of “holiday” where he only had to concentrate on himself. The only problem was when he returned home, he fell back into the addiction cycle.
July
31% of people who said they started between the ages of 15-19, started at 17. This was only for injection drugs, meaning they could have started smoking or alcohol much earlier. Our youngest answer for injecting drugs was 9 years old.
9 Females said 11-14 (8 were Aboriginal/1was Caucasian). 14 Females said 15-19 (12 were Aboriginal/ 2 were Caucasian). 16 Females said 20-24 (11 were Aboriginal/ 5 were Caucasian/ 1 was Other). 5 Females said 25-29 (4 were Aboriginal/ 1 was Caucasian). 4 Females said 30-34 (3 were Aboriginal/ 1 was Caucasian). 3 Females said 35-39 (All were Aboriginal). 2 Females said over 40 (Both were Aboriginal).
1 Male said under 10 (He was Aboriginal). 6 Males said 11-14 (4 were Aboriginal/2 were Caucasian). 22 Males said 15-19 (21 were Aboriginal/ 1 was Caucasian). 16 Males said 20-24 (13 were Aboriginal/ 3 were Caucasian). 8 Males said 25-29 (4 were Aboriginal/ 4 were Caucasian). 4 Males said 30-34 (3 were Aboriginal/ 1 was Caucasian). 1 Male said 35-39 (He was Aboriginal). 4 Males said over 40 (3 were Aboriginal/ 1 was Caucasian).
One lady’s answer stuck with us. “I started when I was 44; when I could make my own bad decisions, unlike my 16 year old granddaughter”. As we can see from our survey, the highest age group starting injection drugs are between 15-19.
Since our database records the year our clients were born, we can calculate the number of years to date a client has been using injection drugs. The average amount is 18 years; with 42 being the highest and just started this year being the lowest. Which offers the question…is it harder to quit drugs the more years you have been hooked or harder to quit when you have just started? (We can’t say for sure if clients have been injecting the entire time ie. incarceration, in treatment, etc)
9 Females said 11-14 (8 were Aboriginal/1was Caucasian). 14 Females said 15-19 (12 were Aboriginal/ 2 were Caucasian). 16 Females said 20-24 (11 were Aboriginal/ 5 were Caucasian/ 1 was Other). 5 Females said 25-29 (4 were Aboriginal/ 1 was Caucasian). 4 Females said 30-34 (3 were Aboriginal/ 1 was Caucasian). 3 Females said 35-39 (All were Aboriginal). 2 Females said over 40 (Both were Aboriginal).
1 Male said under 10 (He was Aboriginal). 6 Males said 11-14 (4 were Aboriginal/2 were Caucasian). 22 Males said 15-19 (21 were Aboriginal/ 1 was Caucasian). 16 Males said 20-24 (13 were Aboriginal/ 3 were Caucasian). 8 Males said 25-29 (4 were Aboriginal/ 4 were Caucasian). 4 Males said 30-34 (3 were Aboriginal/ 1 was Caucasian). 1 Male said 35-39 (He was Aboriginal). 4 Males said over 40 (3 were Aboriginal/ 1 was Caucasian).
One lady’s answer stuck with us. “I started when I was 44; when I could make my own bad decisions, unlike my 16 year old granddaughter”. As we can see from our survey, the highest age group starting injection drugs are between 15-19.
Since our database records the year our clients were born, we can calculate the number of years to date a client has been using injection drugs. The average amount is 18 years; with 42 being the highest and just started this year being the lowest. Which offers the question…is it harder to quit drugs the more years you have been hooked or harder to quit when you have just started? (We can’t say for sure if clients have been injecting the entire time ie. incarceration, in treatment, etc)
August
The “Other” category included wanting to appear older (wanting to fit in), mental health like depression, and wanting a stronger high.
83.3% of people who answered family were Aboriginal descent. An Aboriginal woman who answered our survey specified that her mother taught her how to use.
7 Females said curiosity (all were Aboriginal). 6 Females said family (all were Aboriginal). 7 Females said friends (all were Aboriginal). 2 Females said grief (both were Aboriginal). 6 Females said medical (4 were Aboriginal/ 2 were Caucasian). 2 Females said other (1 was Aboriginal/ 1 was Caucasian)
7 Males said curiosity (6 were Aboriginal/ 1was Caucasian). 6 Males said family (4 were Aboriginal/ 2 were Caucasian). 12 Males said friends (9 were Aboriginal/ 2 were Caucasian/ 1 was Other). 5 Males said some grief (4 were Aboriginal/ 1 was Caucasian). 4 Males said medical (2 were Aboriginal/ 1 was Caucasian/ 1 was Other). 9 Males said other (8 were Aboriginal/ 1 was Caucasian).
Answers ranged from horrific stories of physical or psychological trauma (losing families all at once, residential schools, and missing children) to a man saying his friends bought him drugs as his birthday present (this man answered our last month survey to say he was 16 years old when he first started to inject)
83.3% of people who answered family were Aboriginal descent. An Aboriginal woman who answered our survey specified that her mother taught her how to use.
7 Females said curiosity (all were Aboriginal). 6 Females said family (all were Aboriginal). 7 Females said friends (all were Aboriginal). 2 Females said grief (both were Aboriginal). 6 Females said medical (4 were Aboriginal/ 2 were Caucasian). 2 Females said other (1 was Aboriginal/ 1 was Caucasian)
7 Males said curiosity (6 were Aboriginal/ 1was Caucasian). 6 Males said family (4 were Aboriginal/ 2 were Caucasian). 12 Males said friends (9 were Aboriginal/ 2 were Caucasian/ 1 was Other). 5 Males said some grief (4 were Aboriginal/ 1 was Caucasian). 4 Males said medical (2 were Aboriginal/ 1 was Caucasian/ 1 was Other). 9 Males said other (8 were Aboriginal/ 1 was Caucasian).
Answers ranged from horrific stories of physical or psychological trauma (losing families all at once, residential schools, and missing children) to a man saying his friends bought him drugs as his birthday present (this man answered our last month survey to say he was 16 years old when he first started to inject)
September
25% of people who answered that some people know also said that they hide it from certain people like their family.
44 Females said yes (38 were Aboriginal/ 6 were Caucasian). 7 Females said some people (6 were Aboriginal/ 1 was Caucasian). 7 Females said no (5 were Aboriginal/ 2 were Caucasian)
53 Males said yes (44 were Aboriginal/ 9 were Caucasian). 5 Males said some people (3 were Aboriginal/ 2 were Caucasian). 4 Males said no (All were Aboriginal).
One woman said that other users know of her use but not her boss or coworkers. She is 28 and works in a care home in the city. Another said she makes sure to let her doctors know of her use.
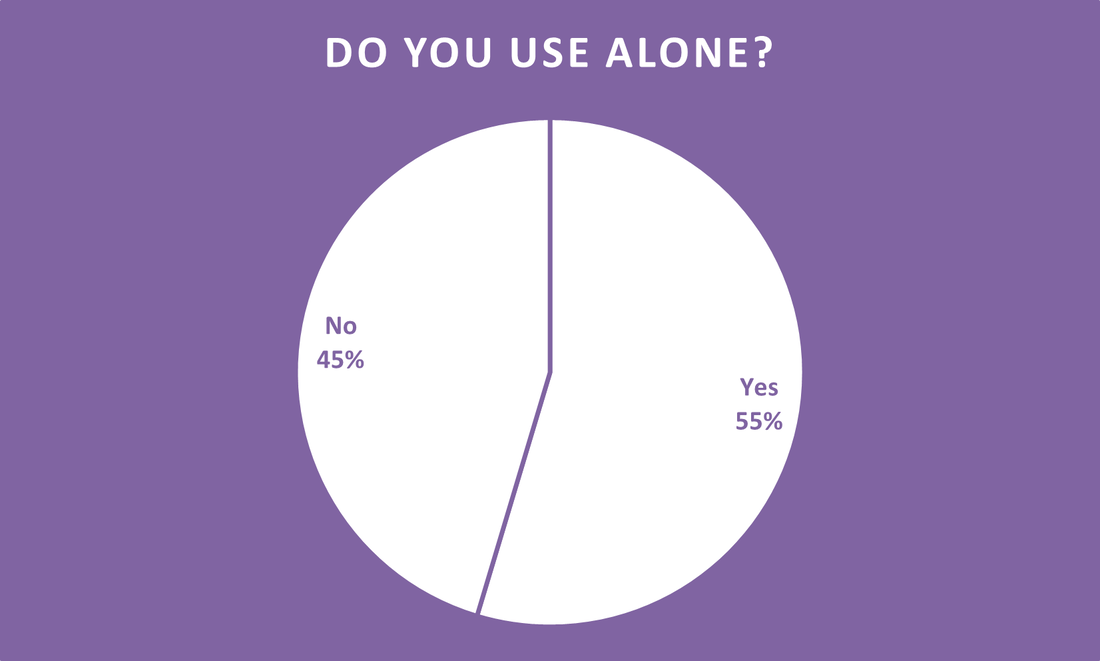
One gentleman said no one knows he uses but there is always someone in the next room in case of emergencies.
With the high rate of overdoses, across Canada with a few happening in Regina, we wanted to make sure clients were aware of not using alone.
44 Females said yes (38 were Aboriginal/ 6 were Caucasian). 7 Females said some people (6 were Aboriginal/ 1 was Caucasian). 7 Females said no (5 were Aboriginal/ 2 were Caucasian)
53 Males said yes (44 were Aboriginal/ 9 were Caucasian). 5 Males said some people (3 were Aboriginal/ 2 were Caucasian). 4 Males said no (All were Aboriginal).
One woman said that other users know of her use but not her boss or coworkers. She is 28 and works in a care home in the city. Another said she makes sure to let her doctors know of her use.
One gentleman said no one knows he uses but there is always someone in the next room in case of emergencies.
With the high rate of overdoses, across Canada with a few happening in Regina, we wanted to make sure clients were aware of not using alone.
October
Of the 24 people who answered yes to overdosing, 16.6% said due to morphine 12.5% said due to Cocaine, 4.2% said due to heroin, 4.2% said due to methadone, 4.2% said to alcohol, and the other 58.3% did not specify. 3 of which have overdosed multiple times, one even said 5 or 6 times, and 3 have died (have been resuscitated).
9 Females said yes (7 were Aboriginal/ 2 were Caucasian). 26 Females said no (25 were Aboriginal/ 1 was Caucasian). 18 Females said knows someone (15 were Aboriginal/ 3 were Caucasian)
15 Males said yes (9 were Aboriginal/ 6 were Caucasian). 26 Males said no (25 were Aboriginal/ 1 was Caucasian).23 Males said knows someone (17 were Aboriginal/ 6 were Caucasian)
One man said he had talked to his doctor after overdosing and was surprised to hear that you can overdose from anything, not just drugs. One woman overdosed on morphine at just 13 years old. We were proud to hear that two of our clients have saved people from overdoses by calling 911 and one even had the training to perform CPR.
On May 4, 2017, the Canadian government made law the Good Samaritan Drug Overdose Act which protects the person experiencing the overdose, the person seeking the help (whether they stay or leave the scene), and anyone else who is at the scene when help arrives from charges for possession of a controlled substance or breach of conditions.
We surveyed an additional amount of people after about their knowledge of the Good Samaritan Drug Overdose Act, 80% of people asked did not know what the act was and 20% heard of the act but did not know it would also protect you from breach of conditions such as probation orders and parole. One woman took a bunch of handouts, saying she knew a lot of people who could benefit from this, and even started talking to people walking into our Needle Exchange about it.
9 Females said yes (7 were Aboriginal/ 2 were Caucasian). 26 Females said no (25 were Aboriginal/ 1 was Caucasian). 18 Females said knows someone (15 were Aboriginal/ 3 were Caucasian)
15 Males said yes (9 were Aboriginal/ 6 were Caucasian). 26 Males said no (25 were Aboriginal/ 1 was Caucasian).23 Males said knows someone (17 were Aboriginal/ 6 were Caucasian)
One man said he had talked to his doctor after overdosing and was surprised to hear that you can overdose from anything, not just drugs. One woman overdosed on morphine at just 13 years old. We were proud to hear that two of our clients have saved people from overdoses by calling 911 and one even had the training to perform CPR.
On May 4, 2017, the Canadian government made law the Good Samaritan Drug Overdose Act which protects the person experiencing the overdose, the person seeking the help (whether they stay or leave the scene), and anyone else who is at the scene when help arrives from charges for possession of a controlled substance or breach of conditions.
We surveyed an additional amount of people after about their knowledge of the Good Samaritan Drug Overdose Act, 80% of people asked did not know what the act was and 20% heard of the act but did not know it would also protect you from breach of conditions such as probation orders and parole. One woman took a bunch of handouts, saying she knew a lot of people who could benefit from this, and even started talking to people walking into our Needle Exchange about it.
November
A qualitative study conducted in 2000 by Rhode Island doctors among injection drug using women in Rhode Island with attitudes toward testing, treatment, and vaccination for hepatitis and HIV, spoke on belonging to a stigmatized group and the perception that medical providers treat injection drug users differently which discouraged some women from seeking testing for HIV and Hepatitis and from seeking treatment. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3291496/#).
We wanted to survey only women but from our everyday stats, only 44.5% of people picking up needles are women. In 2018, we would like to do a survey specifically for women.
25 Females said yes (23 were Aboriginal/ 2 were Caucasian). 14 Females said no (All Aboriginal).
20 Males said yes (17 were Aboriginal/ 3 were Caucasian). 20 Males said no (14 were Aboriginal/ 6 were Caucasian).
One woman first answered no to the question but then went on to say that she is addicted to the drugs her doctors prescribed and now they are racist and rude towards her as an addict. Another three women expressed that doctors treat them differently once they know they use IV drugs; that they don’t listen and they shush you. On a lighter note, many said it is getting better especially in the hospitals, and a couple people said they’ve never been refused services or judged in Regina.
We want our Needle Exchange clients to understand the importance of telling their doctors what they are using and the importance of getting tested for HIV and Hepatitis C. In December, we are asking if our clients have been tested this year as a follow up.
We wanted to survey only women but from our everyday stats, only 44.5% of people picking up needles are women. In 2018, we would like to do a survey specifically for women.
25 Females said yes (23 were Aboriginal/ 2 were Caucasian). 14 Females said no (All Aboriginal).
20 Males said yes (17 were Aboriginal/ 3 were Caucasian). 20 Males said no (14 were Aboriginal/ 6 were Caucasian).
One woman first answered no to the question but then went on to say that she is addicted to the drugs her doctors prescribed and now they are racist and rude towards her as an addict. Another three women expressed that doctors treat them differently once they know they use IV drugs; that they don’t listen and they shush you. On a lighter note, many said it is getting better especially in the hospitals, and a couple people said they’ve never been refused services or judged in Regina.
We want our Needle Exchange clients to understand the importance of telling their doctors what they are using and the importance of getting tested for HIV and Hepatitis C. In December, we are asking if our clients have been tested this year as a follow up.
December
11.7% of all people asked, inquired about testing (compared to the 10.8% from January’s survey). This time 11 of the 14 were Male compared to the majority being Female in January.
32 Females said yes (26 were Aboriginal/ 6 were Caucasian). 15 Females said no (13 were Aboriginal/ 2 were Caucasian)
48 Males said yes (38 were Aboriginal/ 10 were Caucasian). 25 Males said no (19 were Aboriginal/ 6 were Caucasian)
Eight individuals answered our January survey and our December survey (6 Males and 2 Females). Two had been tested for HIV before but did not get tested this year, one had never been tested but got tested this year, and the other 5 had been tested for HIV before and had also gotten tested this year too.
When asked the question, two separate males disclosed their positive status to us. One specified that they were happy to take their medication as it allowed them to be undetectable. Another talked about the importance of getting tested especially when injecting drugs.
32 Females said yes (26 were Aboriginal/ 6 were Caucasian). 15 Females said no (13 were Aboriginal/ 2 were Caucasian)
48 Males said yes (38 were Aboriginal/ 10 were Caucasian). 25 Males said no (19 were Aboriginal/ 6 were Caucasian)
Eight individuals answered our January survey and our December survey (6 Males and 2 Females). Two had been tested for HIV before but did not get tested this year, one had never been tested but got tested this year, and the other 5 had been tested for HIV before and had also gotten tested this year too.
When asked the question, two separate males disclosed their positive status to us. One specified that they were happy to take their medication as it allowed them to be undetectable. Another talked about the importance of getting tested especially when injecting drugs.