In 2018, we surveyed Needle Exchange clients for 3 weeks every month. We asked an anonymous question to 120 different people and then took down their answer and their Needle Exchange ID. This was done to ensure accuracy of results and evade duplicated data. At the end of the three weeks, all data was collected and separated by gender, age, ethnicity, and location. (Graphs were made depending on relevance).
The questions we asked were as followed:
People were very open with their answers, even to the point of going into detail and telling our staff their story. By providing a safe space, being anonymous and having consistent staff, needle exchange clients are more likely to trust us.
From our everyday stats, only 16% of people picking up needles are Caucasian. We make sure to keep that percentage with everyone we ask.
The responses from the injection drug users have been informative which have helped in relationship building as well as enhance our programs to meet the needs of our clients.
In 2019, we will take this data as a needs assessment and turn what we have learned into where we need to focus. This could include: increased youth education on injection drug use, working with our NEP clients in a way they will understand, and creating awareness events for the public.
The questions we asked were as followed:
- January- What do you use needles for? (What drug?)
- February- Do you get tested regularly for STI’s?
- March- How much do you spend on drugs in a week?
- April- When did you start using?
- May- Why did you start using?
- June- Do you own a Naloxone kit?
- July/August- What was your first drug? (Alcohol/Nicotine/Marijuana/Other)
- September- What other methods do you use to get high besides using needles? (snort/huff/smoke/ingest)
- October- Have you overdosed? What on?
- November- Have you ever been to treatment?
- December- Have you been tested for HIV this year?
People were very open with their answers, even to the point of going into detail and telling our staff their story. By providing a safe space, being anonymous and having consistent staff, needle exchange clients are more likely to trust us.
From our everyday stats, only 16% of people picking up needles are Caucasian. We make sure to keep that percentage with everyone we ask.
The responses from the injection drug users have been informative which have helped in relationship building as well as enhance our programs to meet the needs of our clients.
In 2019, we will take this data as a needs assessment and turn what we have learned into where we need to focus. This could include: increased youth education on injection drug use, working with our NEP clients in a way they will understand, and creating awareness events for the public.
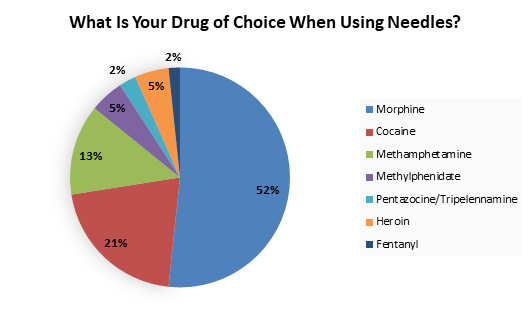
January
24.2% of all people who said morphine specified that they did hydromorphone, which is approximately 5 times stronger than morphine.
27 Females said morphine (26 were Aboriginal/ 1 was Caucasian). 11 Females said cocaine (8 were Aboriginal/ 2 were Caucasian/ 1 was Other). 7 Female said methamphetamine (3 were Aboriginal/ 4 were Caucasian). 4 Females said methylphenidate (All were Aboriginal). 3 Females said pentazocine/ tripelennamine (All were Aboriginal). 1 Female said heroin (She was Aboriginal). 2 Females said Fentanyl (1 was Aboriginal/ 1 was Caucasian).
35 Males said morphine (27 were Aboriginal/ 7 were Caucasian/ 1 was Other). 14 Males said cocaine (11 were Aboriginal/ 2 were Caucasian/ 1 was Other). 9 Males said methamphetamines (6 were Aboriginal/ 3 were Caucasian). 2 Males said methylphenidate (All were Aboriginal). 5 Males said heroin (4 were Aboriginal/ 1 was Caucasian).
Listed on the graph are the medical drug names but in the Needle exchange we received the following drug slang: Down, Side, Sets, T’s and R’s, Coke, Up, and Jib.
In May 2017, reported by CBC News, crystal meth spiked dramatically in Saskatchewan and the health minister said, “Fentanyl has received a lot of attention and certainly the mortality is significant, but what's being missed here is the mortality associated with crystal meth in part due to HIV/AIDS. People with HIV are too unstable to continue the daily treatment they need to survive while using crystal meth.” (http://www.cbc.ca/news/canada/saskatoon/minister-reiter-meth-crisis-response-saskatchewan-1.4138363).
By comparing our results from January 2018 and March 2017, our clients still continue to use morphine and cocaine over crystal meth with only 16 individuals using meth in January and 7 using in March.
27 Females said morphine (26 were Aboriginal/ 1 was Caucasian). 11 Females said cocaine (8 were Aboriginal/ 2 were Caucasian/ 1 was Other). 7 Female said methamphetamine (3 were Aboriginal/ 4 were Caucasian). 4 Females said methylphenidate (All were Aboriginal). 3 Females said pentazocine/ tripelennamine (All were Aboriginal). 1 Female said heroin (She was Aboriginal). 2 Females said Fentanyl (1 was Aboriginal/ 1 was Caucasian).
35 Males said morphine (27 were Aboriginal/ 7 were Caucasian/ 1 was Other). 14 Males said cocaine (11 were Aboriginal/ 2 were Caucasian/ 1 was Other). 9 Males said methamphetamines (6 were Aboriginal/ 3 were Caucasian). 2 Males said methylphenidate (All were Aboriginal). 5 Males said heroin (4 were Aboriginal/ 1 was Caucasian).
Listed on the graph are the medical drug names but in the Needle exchange we received the following drug slang: Down, Side, Sets, T’s and R’s, Coke, Up, and Jib.
In May 2017, reported by CBC News, crystal meth spiked dramatically in Saskatchewan and the health minister said, “Fentanyl has received a lot of attention and certainly the mortality is significant, but what's being missed here is the mortality associated with crystal meth in part due to HIV/AIDS. People with HIV are too unstable to continue the daily treatment they need to survive while using crystal meth.” (http://www.cbc.ca/news/canada/saskatoon/minister-reiter-meth-crisis-response-saskatchewan-1.4138363).
By comparing our results from January 2018 and March 2017, our clients still continue to use morphine and cocaine over crystal meth with only 16 individuals using meth in January and 7 using in March.
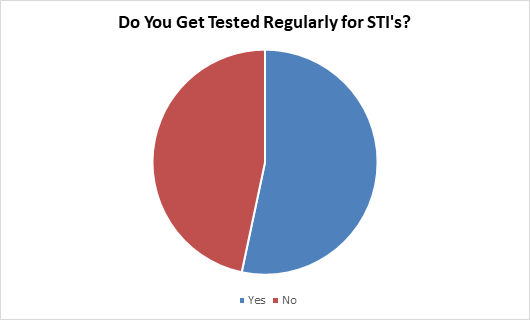
FEBRUARY
19% of people who answered no specified that they were married with the same partner.
18.9% of people participating in our survey practice safe sex through the use of condoms even though 35% of that group answered no to getting tested regularly.
5 women self identified as street workers and all of them said they get tested regularly.
24 Females said yes (20 were Aboriginal/ 3 were Caucasian/ 1 was Other). 17 Females said no (13 were Aboriginal/ 4 were Caucasian)
24 Males said yes (20 were Aboriginal/ 4 were Caucasian). 25 Males said no (19 were Aboriginal/ 6 were Caucasian).
On February 14th, we sent our students to the University of Regina to hand out condoms and promote testing and safer sex. We gave out over 1500 condoms and 500 testing cards. The next day during testing, we had one person come specifically because of our testing promotion the day before.
9 people, in the 3 weeks the survey was being done, were tested for HIV, HCV, and STI’s compared to the month of December (1) and the month of January (5). Unfortunately, our nurse is only in on Thursdays for 2 hours which hinders people getting tested.
18.9% of people participating in our survey practice safe sex through the use of condoms even though 35% of that group answered no to getting tested regularly.
5 women self identified as street workers and all of them said they get tested regularly.
24 Females said yes (20 were Aboriginal/ 3 were Caucasian/ 1 was Other). 17 Females said no (13 were Aboriginal/ 4 were Caucasian)
24 Males said yes (20 were Aboriginal/ 4 were Caucasian). 25 Males said no (19 were Aboriginal/ 6 were Caucasian).
On February 14th, we sent our students to the University of Regina to hand out condoms and promote testing and safer sex. We gave out over 1500 condoms and 500 testing cards. The next day during testing, we had one person come specifically because of our testing promotion the day before.
9 people, in the 3 weeks the survey was being done, were tested for HIV, HCV, and STI’s compared to the month of December (1) and the month of January (5). Unfortunately, our nurse is only in on Thursdays for 2 hours which hinders people getting tested.
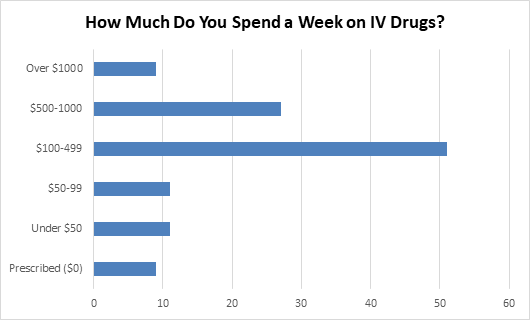
March
On average, the people surveyed spend $431 a week (with an average of $197 in the $100-499 bracket).
5 Females said prescribed (3 were Aboriginal/ 2 were Caucasian). 2 Females said under $50 (both were Aboriginal). 4 Females said between $50-99 (3 were Aboriginal/ 1 was Caucasian). 23 Females said between $100-499 (20 were Aboriginal/ 3 were Caucasian). 10 Females said between $500-1000 (9 were Aboriginal/ 1 was Caucasian). 5 Females said over $1000 (2 were Aboriginal/ 3 were Caucasian).
4 Males said prescribed (3 were Aboriginal/ 1 was Caucasian). 9 Males said under $50 (8 were Aboriginal/ 1 was Caucasian). 7 Males said between $50-99 (all were Aboriginal). 28 Males said between $100-499 (23 were Aboriginal/ 5 were Caucasian). 17 Males said between $500-1000 (13 were Aboriginal/ 4 were Caucasian). 4 Males said over $1000 (3 were Aboriginal/ 1 was Other).
22 people also answered our January survey (What is your drug of choice?) and found that their spending habits were sporadic. 12 said morphine with prices ranging from prescribed ($0) to $900 a week. 4 said cocaine with prices ranging from $100-700 a week. 3 said Ritalin with prices ranging from $60-1,000 a week. 2 said crystal meth with prices ranging from $400-1,100 a week. 1 said heroin for $2,000 a week. From these numbers we are unable to see how many times our clients are using said drug per day however we had 5 people answer our 2017 April survey (How many times do you use a day?) and their answers ranged from twice a day to 5 times.
5 Females said prescribed (3 were Aboriginal/ 2 were Caucasian). 2 Females said under $50 (both were Aboriginal). 4 Females said between $50-99 (3 were Aboriginal/ 1 was Caucasian). 23 Females said between $100-499 (20 were Aboriginal/ 3 were Caucasian). 10 Females said between $500-1000 (9 were Aboriginal/ 1 was Caucasian). 5 Females said over $1000 (2 were Aboriginal/ 3 were Caucasian).
4 Males said prescribed (3 were Aboriginal/ 1 was Caucasian). 9 Males said under $50 (8 were Aboriginal/ 1 was Caucasian). 7 Males said between $50-99 (all were Aboriginal). 28 Males said between $100-499 (23 were Aboriginal/ 5 were Caucasian). 17 Males said between $500-1000 (13 were Aboriginal/ 4 were Caucasian). 4 Males said over $1000 (3 were Aboriginal/ 1 was Other).
22 people also answered our January survey (What is your drug of choice?) and found that their spending habits were sporadic. 12 said morphine with prices ranging from prescribed ($0) to $900 a week. 4 said cocaine with prices ranging from $100-700 a week. 3 said Ritalin with prices ranging from $60-1,000 a week. 2 said crystal meth with prices ranging from $400-1,100 a week. 1 said heroin for $2,000 a week. From these numbers we are unable to see how many times our clients are using said drug per day however we had 5 people answer our 2017 April survey (How many times do you use a day?) and their answers ranged from twice a day to 5 times.
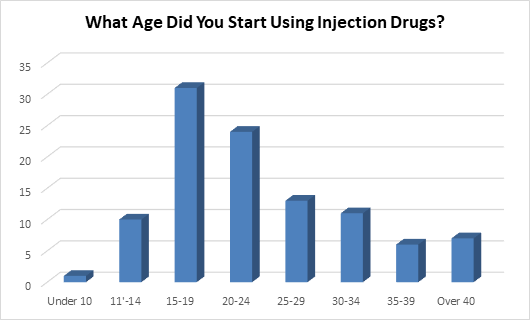
April
32% of people who said they started between the ages of 15-19, started at 19; 29% started at 16. This was only for injection drugs, meaning they could have started smoking or drinking alcohol much earlier. Our youngest answer for injecting drugs was 9 years old.
6 Females said 11-14 years old (4 were Aboriginal/2 were Caucasian). 10 Females said 15-19 years old (All were Aboriginal). 13 Females said 20-24 years old (11 were Aboriginal/2 were Caucasian). 6 Females said 25-29 years old (5 were Aboriginal/ 1 was Caucasian). 4 Females said 30-34 years old (2were Aboriginal/ 2 were Caucasian). 2 Females said 35-39 years old (All were Aboriginal). 4 Females said over 40 years old (All were Aboriginal).
1 Male said under 10 years old (He was Aboriginal). 4 Males said 11-14 years old (2 were Aboriginal/2 were Caucasian). 21 Males said 15-19 years old (18 were Aboriginal/ 3 were Caucasian). 11 Males said 20-24 years old (10 were Aboriginal/1 was Caucasian). 7 Males said 25-29 years old (2 were Aboriginal/ 5 were Caucasian). 7 Males said 30-34 years old (6 were Aboriginal/ 1 was Caucasian). 4 Males said 35-39 years old (3 were Aboriginal/ 1 was Caucasian). 3 Males said over 40 years old (2 were Aboriginal/ 1 was Caucasian).
Since our database records the year our clients were born, we can calculate the number of years to date a client has been using injection drugs. The average amount is 16 years; with 43 being the highest and just started this year being the lowest. Which offers the question…is it harder to quit drugs the more years you have been hooked or harder to quit when you have just started? (We can’t say for sure if clients have been injecting the entire time ie. incarceration, in treatment, etc)
6 Females said 11-14 years old (4 were Aboriginal/2 were Caucasian). 10 Females said 15-19 years old (All were Aboriginal). 13 Females said 20-24 years old (11 were Aboriginal/2 were Caucasian). 6 Females said 25-29 years old (5 were Aboriginal/ 1 was Caucasian). 4 Females said 30-34 years old (2were Aboriginal/ 2 were Caucasian). 2 Females said 35-39 years old (All were Aboriginal). 4 Females said over 40 years old (All were Aboriginal).
1 Male said under 10 years old (He was Aboriginal). 4 Males said 11-14 years old (2 were Aboriginal/2 were Caucasian). 21 Males said 15-19 years old (18 were Aboriginal/ 3 were Caucasian). 11 Males said 20-24 years old (10 were Aboriginal/1 was Caucasian). 7 Males said 25-29 years old (2 were Aboriginal/ 5 were Caucasian). 7 Males said 30-34 years old (6 were Aboriginal/ 1 was Caucasian). 4 Males said 35-39 years old (3 were Aboriginal/ 1 was Caucasian). 3 Males said over 40 years old (2 were Aboriginal/ 1 was Caucasian).
Since our database records the year our clients were born, we can calculate the number of years to date a client has been using injection drugs. The average amount is 16 years; with 43 being the highest and just started this year being the lowest. Which offers the question…is it harder to quit drugs the more years you have been hooked or harder to quit when you have just started? (We can’t say for sure if clients have been injecting the entire time ie. incarceration, in treatment, etc)
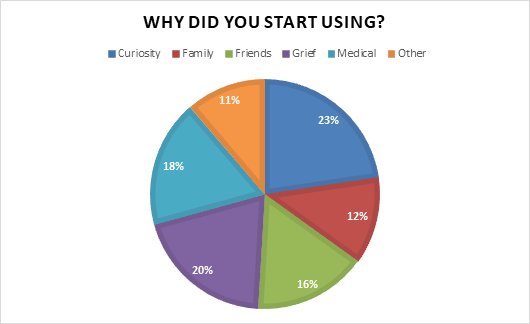
May
The “Other” category included something to do in jail, wanting to quit drinking and wanting a stronger high.
48% of people who answered grief also mentioned that they continue to use due to mental health issues such as depression and feeling suicidal.
10 Females said Curiosity (9 were Aboriginal/ 1 was Caucasian). 8 Females said Family (All were Aboriginal). 8 Females said Friends (6 were Aboriginal/ 2 were Caucasian). 15 Females said Grief (13 were Aboriginal/ 2 were Caucasian). 8 Females said Medical (All were Aboriginal). 5 Females said Other (2 were Aboriginal/ 3 were Caucasian).
14 Males said Curiosity (11 were Aboriginal/ 3 were Caucasian). 5 Males said Family (All were Aboriginal). 9 Males said Friends (8 were Aboriginal/ 1 was Caucasian). 6 Males said Grief (3 were Aboriginal/ 3 were Caucasian). 11 Males said Medical (5 were Aboriginal/ 6 were Caucasian). 7 Males said Other (4 were Aboriginal/ 3 were Caucasian).
Answers ranged from horrific stories of physical or psychological trauma (losing loved ones, children being taken away, and sexual assault) to a man saying his family injected him without consent while he was sleeping as it was a “family tradition”.
48% of people who answered grief also mentioned that they continue to use due to mental health issues such as depression and feeling suicidal.
10 Females said Curiosity (9 were Aboriginal/ 1 was Caucasian). 8 Females said Family (All were Aboriginal). 8 Females said Friends (6 were Aboriginal/ 2 were Caucasian). 15 Females said Grief (13 were Aboriginal/ 2 were Caucasian). 8 Females said Medical (All were Aboriginal). 5 Females said Other (2 were Aboriginal/ 3 were Caucasian).
14 Males said Curiosity (11 were Aboriginal/ 3 were Caucasian). 5 Males said Family (All were Aboriginal). 9 Males said Friends (8 were Aboriginal/ 1 was Caucasian). 6 Males said Grief (3 were Aboriginal/ 3 were Caucasian). 11 Males said Medical (5 were Aboriginal/ 6 were Caucasian). 7 Males said Other (4 were Aboriginal/ 3 were Caucasian).
Answers ranged from horrific stories of physical or psychological trauma (losing loved ones, children being taken away, and sexual assault) to a man saying his family injected him without consent while he was sleeping as it was a “family tradition”.
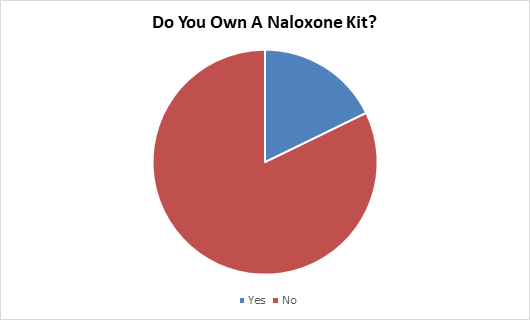
June
60% of people who answered no inquired about training and receiving a kit.
11 Females said yes (7 were Aboriginal/ 4 were Caucasian). 39 Females said no (33 were Aboriginal/ 6 were Caucasian)
10 Males said yes (8 were Aboriginal/ 1 was Caucasian/ 1 was Other). 58 Males said no (46 were Aboriginal/ 11 were Caucasian/ 1 was Other).
With the high levels of interest in Naloxone kits and training, AIDS Programs South Saskatchewan (APSS) became a distribution site in November 2018. All APSS staff have been trained and will be able to train anyone interested in Naloxone. The training, depending on those being trained, takes 30 minutes and trains individuals on how to administer the drug, how to identify an overdose, and overdose prevention. Kits can be distributed to injection drug users or family of injection drug users who have taken the training.
From November to December 2018, 7 people were trained with 1 people being eligible to receive a kit. In 2019, we are aiming to double these numbers through more promotion in our needle exchange and off-site training of health care professionals.
11 Females said yes (7 were Aboriginal/ 4 were Caucasian). 39 Females said no (33 were Aboriginal/ 6 were Caucasian)
10 Males said yes (8 were Aboriginal/ 1 was Caucasian/ 1 was Other). 58 Males said no (46 were Aboriginal/ 11 were Caucasian/ 1 was Other).
With the high levels of interest in Naloxone kits and training, AIDS Programs South Saskatchewan (APSS) became a distribution site in November 2018. All APSS staff have been trained and will be able to train anyone interested in Naloxone. The training, depending on those being trained, takes 30 minutes and trains individuals on how to administer the drug, how to identify an overdose, and overdose prevention. Kits can be distributed to injection drug users or family of injection drug users who have taken the training.
From November to December 2018, 7 people were trained with 1 people being eligible to receive a kit. In 2019, we are aiming to double these numbers through more promotion in our needle exchange and off-site training of health care professionals.
July/August
The Other category included prescription drugs, such as ADHD medication and pain medication, and illegal drugs, such as cocaine, LSD, and ecstasy.
43% of the people who answered other said their first drug was cocaine even after explaining the definition of a drug (“a substance which has a physiological effect when ingested or otherwise introduced into the body”). However, many who were asked the survey question did not view nicotine or alcohol as a drug.
3 Females said alcohol (2 were Aboriginal/ 1 was Caucasian). 10 Females said marijuana (9 were Aboriginal/ 1 was Caucasian). 8 Females said nicotine (5 were Aboriginal/ 3 were Caucasian). 10 Females said other (7 were Aboriginal/ 3 were Caucasian).
7 Males said alcohol (3 were Aboriginal/ 4 were Caucasian). 9 Males said marijuana (6 were Aboriginal/ 3 were Caucasian). 8 Males said nicotine (7 were Aboriginal/ 1 was Caucasian). 5 Males said other (3 were Aboriginal/ 2 was Caucasian).
One woman told us that she started on nicotine because everyone was smoking, and it was easily accessible. She then started “real drugs” when she was 26 years old (33 years ago). One man described his drug journey as he got older, starting with alcohol and then marijuana, cocaine, and crystal meth. One man was nine years old when his older brother showed him how to inject cocaine. The youngest we had using a drug was seven years old (this was on marijuana).
43% of the people who answered other said their first drug was cocaine even after explaining the definition of a drug (“a substance which has a physiological effect when ingested or otherwise introduced into the body”). However, many who were asked the survey question did not view nicotine or alcohol as a drug.
3 Females said alcohol (2 were Aboriginal/ 1 was Caucasian). 10 Females said marijuana (9 were Aboriginal/ 1 was Caucasian). 8 Females said nicotine (5 were Aboriginal/ 3 were Caucasian). 10 Females said other (7 were Aboriginal/ 3 were Caucasian).
7 Males said alcohol (3 were Aboriginal/ 4 were Caucasian). 9 Males said marijuana (6 were Aboriginal/ 3 were Caucasian). 8 Males said nicotine (7 were Aboriginal/ 1 was Caucasian). 5 Males said other (3 were Aboriginal/ 2 was Caucasian).
One woman told us that she started on nicotine because everyone was smoking, and it was easily accessible. She then started “real drugs” when she was 26 years old (33 years ago). One man described his drug journey as he got older, starting with alcohol and then marijuana, cocaine, and crystal meth. One man was nine years old when his older brother showed him how to inject cocaine. The youngest we had using a drug was seven years old (this was on marijuana).
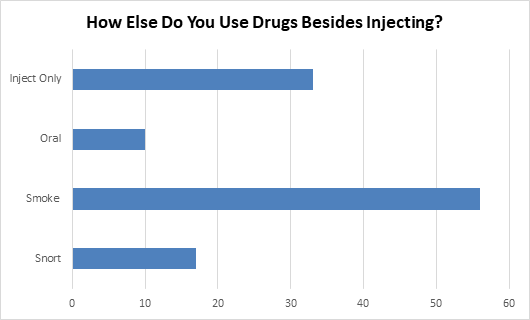
September
16 of the 116 asked said not only do they inject drugs, they also smoke, snort, take orally, and sometimes huff.
14 Females said inject only (12 were Aboriginal/ 1 was Caucasian/ 1 was Other). 3 Females said oral (All were Aboriginal). 34 Females said smoke (26 were Aboriginal/ 8 were Caucasian). 7 Females said snort (5 were Aboriginal/ 2 were Caucasian).
19 Males said inject only (15 were Aboriginal/ 3 were Caucasian/ 1 was Other). 7 Males said oral (5 were Aboriginal/ 1 was Caucasian/ 1 was Other). 22 Males said smoke (18 were Aboriginal/ 4 were Caucasian). 10 Males said snort (3 were Aboriginal/ 7 were Caucasian).
One man used to “do it all” but now is slowly quitting by only injecting while another man is switching to a different method to consume drugs instead of injecting. One man, since he was nine years old (24 years ago), has been only injecting.
In August, AIDS Saskatoon pushed for clean pipes to be supplied at needle exchanges across Saskatchewan in an effort to reduce HIV rates. The hope was that injection drug users would use them to get high instead of needles if pipes were more available. After talks across the province, pipes will be available at needle exchanges March 2019.
14 Females said inject only (12 were Aboriginal/ 1 was Caucasian/ 1 was Other). 3 Females said oral (All were Aboriginal). 34 Females said smoke (26 were Aboriginal/ 8 were Caucasian). 7 Females said snort (5 were Aboriginal/ 2 were Caucasian).
19 Males said inject only (15 were Aboriginal/ 3 were Caucasian/ 1 was Other). 7 Males said oral (5 were Aboriginal/ 1 was Caucasian/ 1 was Other). 22 Males said smoke (18 were Aboriginal/ 4 were Caucasian). 10 Males said snort (3 were Aboriginal/ 7 were Caucasian).
One man used to “do it all” but now is slowly quitting by only injecting while another man is switching to a different method to consume drugs instead of injecting. One man, since he was nine years old (24 years ago), has been only injecting.
In August, AIDS Saskatoon pushed for clean pipes to be supplied at needle exchanges across Saskatchewan in an effort to reduce HIV rates. The hope was that injection drug users would use them to get high instead of needles if pipes were more available. After talks across the province, pipes will be available at needle exchanges March 2019.
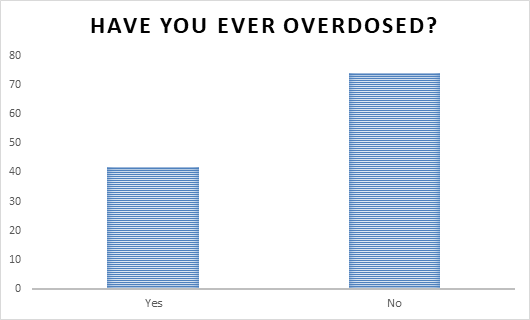
october
Of the 42 people who answered yes (an increase of 75% from last years survey (from 24 to 42)) to overdosing, 7.1% said due to crystal meth, 26.2% said due to cocaine,14.3% said due to fentanyl, 33.3% said due to heroin, 4.8% said due to methadone, and the other 14.3% amounted to painkillers, alcohol and pills.
8 have overdosed multiple times, one even said 9 times on heroin alone, and 2 have died (have been resuscitated or been in a coma).
19 Females said yes (All were Aboriginal). 36 Females said no (32 were Aboriginal/4 were Caucasian).
23 Males said yes (15 were Aboriginal/8 were Caucasian). 38 Males said no (27 were Aboriginal/9 were Caucasian/2 were Other).
One woman said that for the twenty-three years she has been using injection drugs, since she was seventeen years old, she has never overdosed. However, she also was a morphine user who was not using harder drugs that our clients are overdosing on such as heroin, cocaine, or fentanyl. One man overdosed on painkillers while selling in a gang when he was young. One man overdosed in Vancouver where a naloxone kit saved him.
We continue to educate our clients in the needle exchange with quick informative tips and handbills. Information includes harm reduction such as overdose prevention, HIV information on down to reduce the spread of HIV, STI information and where to get tested, and addiction information for treatment. This year, 2,311 conversations were made with 700 in relation to harm reduction.
8 have overdosed multiple times, one even said 9 times on heroin alone, and 2 have died (have been resuscitated or been in a coma).
19 Females said yes (All were Aboriginal). 36 Females said no (32 were Aboriginal/4 were Caucasian).
23 Males said yes (15 were Aboriginal/8 were Caucasian). 38 Males said no (27 were Aboriginal/9 were Caucasian/2 were Other).
One woman said that for the twenty-three years she has been using injection drugs, since she was seventeen years old, she has never overdosed. However, she also was a morphine user who was not using harder drugs that our clients are overdosing on such as heroin, cocaine, or fentanyl. One man overdosed on painkillers while selling in a gang when he was young. One man overdosed in Vancouver where a naloxone kit saved him.
We continue to educate our clients in the needle exchange with quick informative tips and handbills. Information includes harm reduction such as overdose prevention, HIV information on down to reduce the spread of HIV, STI information and where to get tested, and addiction information for treatment. This year, 2,311 conversations were made with 700 in relation to harm reduction.
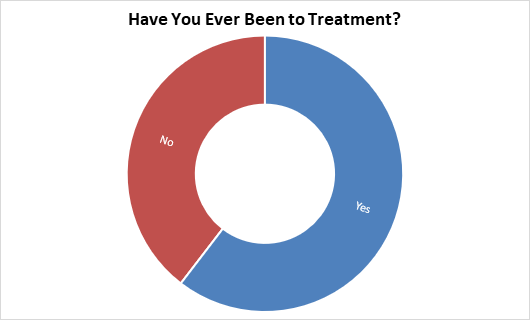
November
13 people were referred to treatment options in November while asking this survey.
25 Females said yes (22 were Aboriginal/ 3 were Caucasian). 19 Females said no (17 were Aboriginal/ 2 were Caucasian).
33 Males said yes (23 were Aboriginal/ 10 were Caucasian). 19 Males said no (16 were Aboriginal/ 3 were Caucasian).
6 people had been to treatment more than once (up to five times) and one man had just gotten out of treatment this morning before coming to pick up needles. 3 men had been forced into treatment/detox while in jail and one woman was passionately against treatment and going. She did not believe it worked nor had any interest in attending.
Many who answered yes to this survey said even though they had gone to a treatment centre, they were not ready to quit. As answered in a previous survey, many use drugs because of underlining issues that can not always be treated in one treatment session such as grief, mental health, and family cycles.
25 Females said yes (22 were Aboriginal/ 3 were Caucasian). 19 Females said no (17 were Aboriginal/ 2 were Caucasian).
33 Males said yes (23 were Aboriginal/ 10 were Caucasian). 19 Males said no (16 were Aboriginal/ 3 were Caucasian).
6 people had been to treatment more than once (up to five times) and one man had just gotten out of treatment this morning before coming to pick up needles. 3 men had been forced into treatment/detox while in jail and one woman was passionately against treatment and going. She did not believe it worked nor had any interest in attending.
Many who answered yes to this survey said even though they had gone to a treatment centre, they were not ready to quit. As answered in a previous survey, many use drugs because of underlining issues that can not always be treated in one treatment session such as grief, mental health, and family cycles.
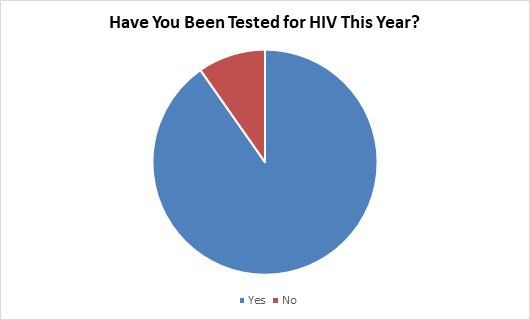
December
In the 3 weeks the survey was being done, 6 people inquired and were referred, with 4 returning for our Thursday HIV testing compared to the month of November (2) and the month of October (4). Unfortunately, our nurse was not in for the 3 weeks and is only normally in on Thursdays for 2 hours which hinders people getting tested.
45 Females said yes (38 were Aboriginal/7 were Caucasian). 3 Females said no (All were Aboriginal).
57 Males said yes (41 were Aboriginal/15 were Caucasian/1 was Other). 8 Males said no (6 were Aboriginal/ 2 were Caucasian).
One man told us he had just got tested as he had gotten bitten. While he had been working security at a local bar, he had been bitten by someone. We assured the man that while this was not an effective route of transmitting HIV, it was a smart idea to get tested. Many people who answered also told us their HIV status which further promotes talking about HIV and breaking down the stigma.
While asking the question, 262 HIV conversations were had on why to get tested, how the test works, and where to get tested.
45 Females said yes (38 were Aboriginal/7 were Caucasian). 3 Females said no (All were Aboriginal).
57 Males said yes (41 were Aboriginal/15 were Caucasian/1 was Other). 8 Males said no (6 were Aboriginal/ 2 were Caucasian).
One man told us he had just got tested as he had gotten bitten. While he had been working security at a local bar, he had been bitten by someone. We assured the man that while this was not an effective route of transmitting HIV, it was a smart idea to get tested. Many people who answered also told us their HIV status which further promotes talking about HIV and breaking down the stigma.
While asking the question, 262 HIV conversations were had on why to get tested, how the test works, and where to get tested.